Gastroesophageal Reflux Disease (GERD), also known as Gastro-Oesophageal Reflux Disease (GORD), is a common yet often underestimated condition that arises when stomach acid or bile repeatedly flows back into the oesophagus, leading to irritation and inflammation of the delicate oesophageal lining [1].
GERD is one of the most frequently reported chronic digestive conditions in the UK [2]. According to research, about 20% of the adult UK population experiences severe acid reflux symptoms consistent with GERD [2], and approximately five new cases are diagnosed per 1,000 people annually [3].
This rising incidence is strongly linked to increasing obesity rates, more sedentary lifestyles, and the widespread adoption of Westernised diets rich in fats, sugars, and processed foods [4][5][6][7]. In fact, studies have shown that urban living and ageing populations further contribute to higher rates of GERD, with women and older adults reporting more frequent and severe symptoms [6].
Globally, GERD presents a significant healthcare challenge, with an estimated prevalence of up to 14% worldwide [8]. In Western countries, this rises to about one in four individuals experiencing recurrent reflux symptoms each year [9].
This variability in prevalence is attributed to differences in diet, obesity prevalence, lifestyle practices, and diagnostic criteria used in studies across regions. Research reveals that younger adults (especially those within the age range of 30-39 years), who traditionally had lower GERD prevalence, are increasingly affected due to lifestyle changes, including poorer diet and physical inactivity [10].
Collectively, the numbers tell a story of how GERD is not only common, but also growing in frequency – reinforcing the importance of effective management strategies.
Understanding GERD as a Condition Impacting QoL
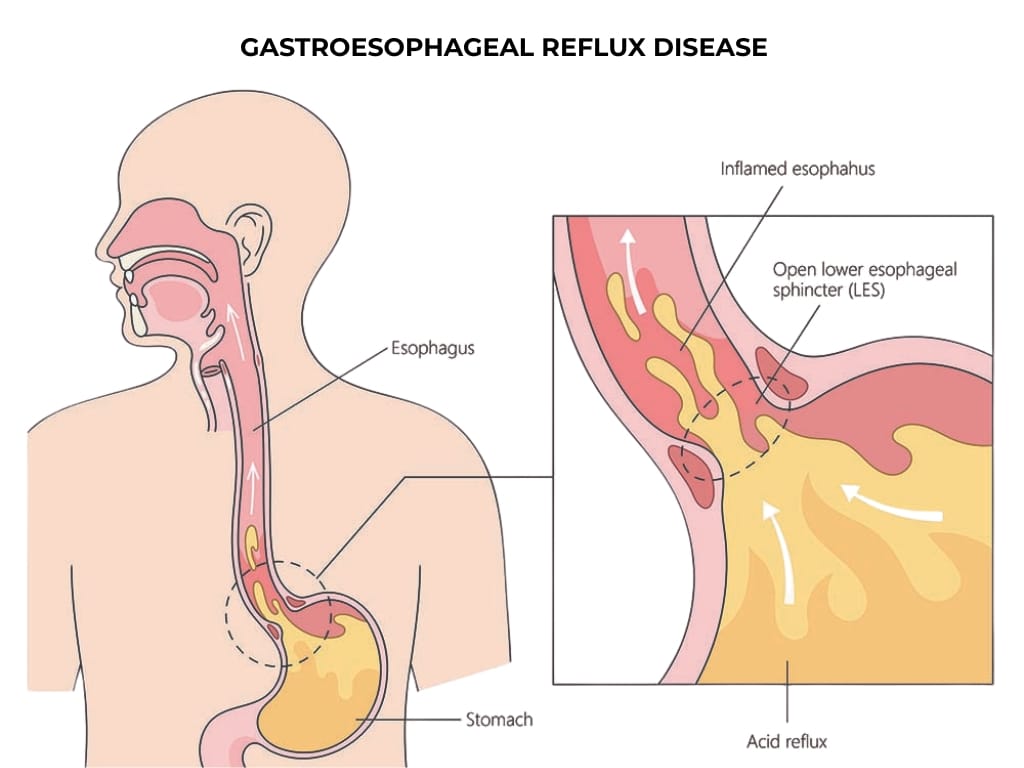
GERD results from the malfunction of the lower oesophageal sphincter (LES), a muscular valve that normally prevents stomach acid from flowing back into the oesophagus. When this sphincter relaxes inappropriately or is weakened, reflux of acid causes symptoms like heartburn, regurgitation, and chest discomfort [11][12].
While occasional heartburn is common and often benign, GERD is characterised by recurrent, troublesome symptoms occurring at least twice a week [13], disrupting everyday life and potentially leading to complications such as oesophageal damage or respiratory issues.
Symptoms can extend beyond heartburn; individuals may experience regurgitation of sour fluid, difficulty swallowing, chronic cough, sore throat, or even dental erosion due to persistent acid exposure [11]. Then, chronic GERD can lead to complications like oesophageal ulcers, strictures, or Barrett’s oesophagus, which carry further health risks and require ongoing medical management, adding to the emotional and financial burden.
Studies consistently reveal that GERD has a profound and multi-dimensional effect on quality of life (QoL) [14][15][16]. Research has found that individuals with GERD report significantly lower scores in physical and mental health, social relationships, and productivity compared with those without GERD, with many experiencing symptoms for over three years.
This chronicity and symptom burden correlated with reduced well-being across all domains, showing GERD’s pervasive impact beyond mere physical discomfort. A 2020 study, for example, highlighted that GERD reduced quality of life scores by nearly 50%, with many individuals struggling with pain, poor sleep, and limited daily activities [15]. In fact, more than 60% reported that their symptoms regularly interfered with work, social life, or emotional well-being [15].
Additional studies reinforce this picture and contribute to a landscape that shows how GORD markedly reduces not just physical health but emotional resilience and social functioning.
Recognising the Triggers for GERD
GERD can be triggered or worsened by a complex combination of dietary, lifestyle, and physiological factors.
Foods commonly consumed across the UK, such as high-fat meals, fried foods, chocolate, peppermint, alcohol, caffeine, and spicy or acidic dishes, are all known to relax the LES or irritate the oesophageal lining, increasing the risk and severity of reflux episodes [17]. Compounding this is the fact that in the UK, obesity rates are rising steadily; over 28% of adults are classified as obese [18], which significantly amplifies the likelihood of developing GERD up to twofold due to increased intra-abdominal pressure pushing stomach acid upward [19].
Lifestyle habits prevalent in the UK also contribute substantially to GERD risk. Smoking rates, while declining, remain significant in certain demographics, and studies show that smoking exacerbates recurrent reflux because nicotine interferes with the LES’s ability to close. Yet the impacts of quitting smoking can be just as profound as a study of 141 former smokers found that almost 44% reported fewer GERD symptoms one year after quitting [20].
Likewise, stress levels, common in the fast-paced modern lifestyle, can provoke or exacerbate GERD symptoms. A 2023 study found that people with moderate to high stress were nearly twice as likely to experience acid reflux symptoms compared to those with low stress. Higher stress was linked to more frequent symptoms such as heartburn, regurgitation, chest pain, cough, and burping [21].
Making Nutrition Part of Management
While medications like proton pump inhibitors and H2 blockers are effective for many and commonly prescribed, research increasingly shows that effective management does not rely solely on medication. Nutritional and behavioural interventions, when personalised and adhered to, can substantially reduce symptom severity and frequency while improving QoL.
Low-carbohydrate diets have been found to reduce oesophageal acid exposure by a mean difference of 2.8%, while high-fibre, plant-forward eating patterns improve stomach motility and decrease pressure-related reflux events [22]. In contrast, high-fat Western diets correlate strongly with increased reflux severity, particularly when combined with sedentary lifestyle behaviours or stress-induced eating [4][5][6][7].
The evidence is clear that diet has a meaningful impact. In a 2025 prospective study involving 47 adults, adherence to a four-week guided diet intervention reduced symptom frequency and severity by more than 60%, alongside measurable improvements in mood, sleep quality, and social wellbeing [23].
Emerging research highlights the close link between the gut and the brain, often referred to as the gut–brain axis. Similar to what is seen with other gastrointestinal diseases like IBS, this is where stress, anxiety, and disrupted sleep can influence gut motility and acid production, amplifying GERD symptoms even when diet remains unchanged [24].
Applying Nutritionist-Led Dietary Strategies and Lifestyle Adjustments
Nutritionists can help individuals living with GERD by identifying individual triggers, while also tailoring meal patterns that reduce stomach pressure and acid stimulation.
Instead of emphasising exclusion, they focus on structure and moderation. Smaller, more frequent meals spaced evenly throughout the day help prevent over-distension of the stomach, while early evening dining – at least three hours before bedtime – minimises nocturnal reflux.
Healthy dietary swaps can make substantial differences. Reducing fried foods and replacing them with grilled or steamed alternatives supports smoother digestion. Substituting acidic or carbonated beverages with water or herbal teas (such as chamomile or ginger) provides additional symptomatic relief. Soluble fibre from foods like oats, bananas, beans, and vegetables helps regulate bowel motility and stabilise gut pressure, while probiotic-rich foods can improve upper GI microbial balance, reducing inflammation and supporting long-term resilience.
Additionally, Mediterranean-style diets, rich in fruits, pulses, olive oil, and seafood, have been linked to a lower risk of reflux-related symptoms [25]. And plant-based diets demonstrate anti-inflammatory effects that protect the oesophageal mucosa and support weight management, too [26]
In a similar vein, weight reduction remains one of the most powerful non-pharmacological tools for GERD. Nutritionists support this through structured meal pacing, balanced energy intake, and incorporation of gentle exercises such as walking or yoga, which both improve gut motility and reduce intra-abdominal pressure. Coupling these changes with other manageable approaches like mindful eating – slowing down, chewing thoroughly, and eating away from screens – reduces food-related reflux further.
Incorporating stress-management techniques such as deep breathing, mindfulness, gentle yoga, and consistent sleep routines can support these changes and improve digestive comfort. Alongside dietary guidance, these stress-reducing behavioural techniques can help individual clients break the cycle of stress-induced reflux and restore a calmer, more balanced digestive rhythm that supports both physical and emotional wellbeing.
Managing GERD With The Health Suite
Ultimately, effective GERD management requires a considered, long-term approach.
While some individuals might see complete symptom resolution with diet and lifestyle adjustments, others may need ongoing medical therapy, particularly in more severe cases. The ultimate goal is always to improve QoL – restoring restful sleep, confidence during meals, and social participation. The Health Suite is primed to support this.
Here at The Health Suite Leicester, clients benefit from a multidisciplinary approach. Initial assessments identify trigger foods and lifestyle factors, which are then addressed through personalised dietary plans, behavioural coaching, and medical oversight if necessary. This tailored strategy ensures that manageable lifestyle changes are sustainable, adaptable, and aligned with each individual’s preferences and circumstances.
Key to this success is education and ongoing support. As individuals learn to identify their personal triggers and develop coping strategies, they regain control over their health. Nutritional guidance offers not just symptom relief but also a pathway to a healthier, more vibrant life – free from the constant worry of reflux episodes, allowing individuals to engage more fully in their daily activities.
In this way, our nutritionist-led support empowers individuals with practical, sustainable strategies and behavioural modifications, creating a foundation for lasting health, reducing dependence on medication and preventing long-term complications. With expert guidance, managing GERD becomes a pathway back to vitality, comfort, and renewed QoL.
Discover how The Health Suite’s personalised, multidisciplinary approach can support your journey toward better health and QoL in Diet & Nutrition Services at The Health Suite Leicester.
Boost your health and wellbeing with personalised Diet & Nutrition support.
References:
- NHS Inform. Gastro-oesophageal reflux disease (GORD). Available at: https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/gastro-oesophageal-reflux-disease-gord/
- Reflux UK. Gastroesophageal Reflux Disease. Available at: https://refluxuk.com/diagnosis/gerd?srsltid=AfmBOop7E9ySf_h230cud920wBbKpbLu07PkwtfsArak10ETjcHqwB7N
- El-Serag HB, et al. Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63(6):871-80
- Alqahtani NS. The Effectiveness of Dietary Intervention in Managing Gastroesophageal Reflux Symptoms: A Prospective Study. Journal of Pioneering Medical Sciences. 2025 Jun;14(6):154-162
- Herdiana Y. Functional Food in Relation to Gastroesophageal Reflux Disease (GERD). Nutrients. 2023;15(16):3583
- Sadafi, S., et al. Risk factors for gastroesophageal reflux disease: a population-based study. BMC Gastroenterol. 2024; 24: 64
- Özenoğlu, A., Anul, N., & Özçelikçi, B. The relationship of gastroesophageal reflux with nutritional habits and mental disorders. Human Nutrition & Metabolism. 2023; 33, 200203
- Kazakova, T, et al. Gastro-esophageal reflux disease in primary care practice: A narrative review. Annals of Esophagus. 2023; 6, 25
- Li, N, et al. Burden of gastroesophageal reflux disease in 204 countries and territories, 1990–2019: A systematic analysis for the Global Burden of Disease Study 2019. BMC Public Health. 2023; 23, 582
- Yamasaki T, et al. The Changing Epidemiology of Gastroesophageal Reflux Disease: Are Patients Getting Younger? J Neurogastroenterol Motil. 2018 Oct 1;24(4):559-569
- Azer SA, Goosenberg E. Gastroesophageal Reflux Disease (GERD). In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025. Available at: https://www.ncbi.nlm.nih.gov/books/NBK554462/
- Healthline. Everything You Need to Know About Acid Reflux and GERD. Available at: https://www.healthline.com/health/gerd
- Chhabra P, Ingole N. Gastroesophageal Reflux Disease (GERD): Highlighting Diagnosis, Treatment, and Lifestyle Changes. Cureus. 2022; 29;14(8):e28563
- Mari, A, et al. Quality of life and severity of symptoms among patients with various degrees of reflux esophagitis: a prospective study. Sci Rep. 2023; 13, 13970
- Alshammari SA, et al. The Determinants of the Quality of Life of Gastroesophageal Reflux Disease Patients Attending King Saud University Medical City. Cureus. 2020; 1;12(8):e9505
- Alomair O, et al. Impact of Gastroesophageal Reflux Disease (GERD) Symptoms on the Lifestyle and Academic Performance of Medical Students at King Faisal University. Cureus. 2023;15(12):e51261
- Healthline. What Foods Should You Avoid with Acid Reflux (Heartburn)? Available at: https://www.healthline.com/health/gerd/foods-to-avoid
- House of Commons Library. Obesity statistics. Available at: https://researchbriefings.files.parliament.uk/documents/SN03336/SN03336.pdf
- El-Serag H. The association between obesity and GERD: a review of the epidemiological evidence. Dig Dis Sci. 2008;53(9):2307-12
- Kohata Y, et al. Long-Term Benefits of Smoking Cessation on Gastroesophageal Reflux Disease and Health-Related Quality of Life. PLoS One. 2016; 11(3): e0150554
- Wickramasinghe N, et al. The association between symptoms of gastroesophageal reflux disease and perceived stress: A countrywide study of Sri Lanka. PLoS One. 2023 Nov 9;18(11):e0294135
- Lakananurak N, et al. The Efficacy of Dietary Interventions in Patients with Gastroesophageal Reflux Disease: A Systematic Review and Meta-Analysis of Intervention Studies. Nutrients. 2024; 5;16(3):464
- Alqahtani, N.S. The Effectiveness of Dietary Intervention in Managing Gastroesophageal Reflux Symptoms: A Prospective Study. Journal of Pioneering Medical Sciences. 2025; 14(6), 154-162
- Caldart F, et al. Overlap of Esophageal Disorders of Gut-Brain Interactions and Gastroesophageal Reflux Disease Is Highly Prevalent in Patients With Refractory Reflux Symptoms. Am J Gastroenterol. 2025 May 22;120(8):1770-1778
- Pharmacy Times. Mediterranean Diet Provides Similar Benefits as Reflux Drugs. Available at: https://www.pharmacytimes.com/view/mediterranean-diet-provides-similar-benefits-as-reflux-drugs
- El Shikieri A, et al. Associations of Plant-Based Foods, Animal Products, and Selected Sociodemographic Factors with Gastroesophageal Reflux Disease Risk. Int. J. Environ. Res. Public Health. 2024, 21, 1696
