We’ve all experienced it: the “gut feeling” before making a decision, or the butterflies in your stomach or gut when you’re nervous. But these sensations are more than just figures of speech – they’re signs of the gut–brain connection at work.
They’re not separate systems. The brain and gut are in constant communication with each other, and at the centre of that conversation is the microbiome, which is a community of trillions of bacteria, fungi, and other microorganisms that live within your digestive system.
It’s currently a trending topic in the wellness space, and science is slowly catching up with the importance of the gut microbiome for our overall health.
At The Health Suite Leicester, many of our patients come in with symptoms like anxiety and brain fog that can be traced back, at least in part, to what’s happening in the gut.
So how does this relationship work, and more importantly, what can you do to support it?
The Gut-Brain Axis
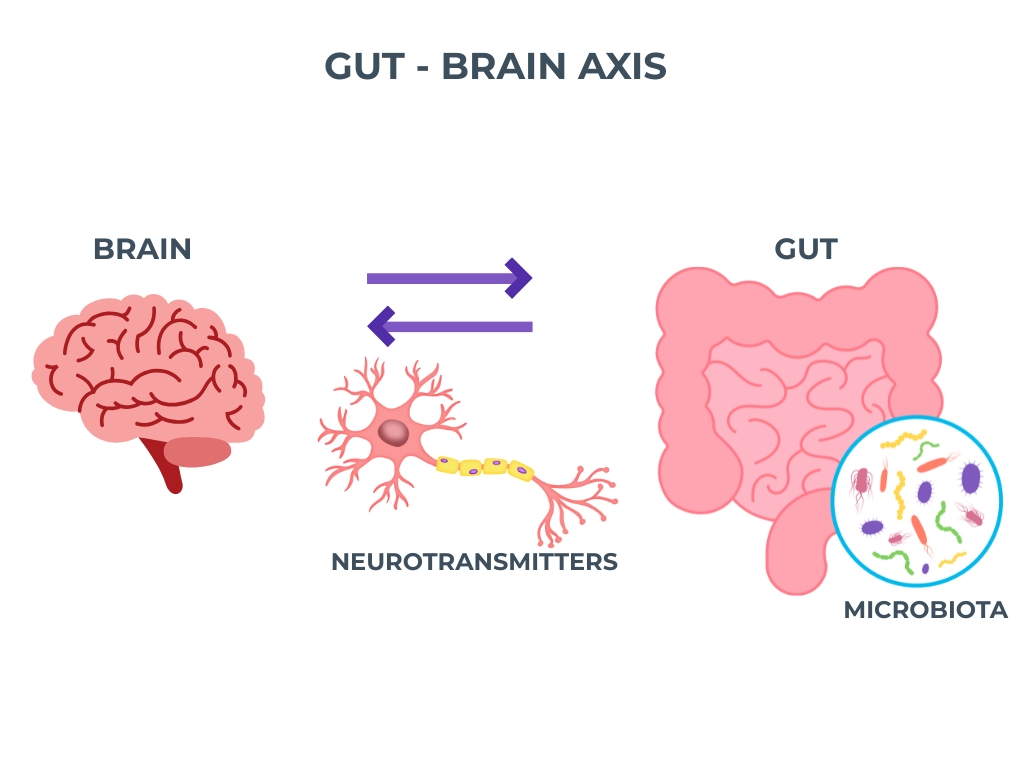
Communication between the gut and brain happens through a network known as the gut–brain axis. And it involves:
- The vagus nerve, which is a centre of information connecting the gut and the brain.
- Immune system signalling, since much of the body’s immune activity begins in the gut.
- Hormones and neurotransmitters, which can be influenced by gut bacteria and impact mood.
So to put it simply, the gut isn’t only there to digest food – it’s actually also sending messages to your brain, affecting how you think, feel, and respond to stress.
Irritable Bowel Syndrome & Mental Health
Irritable Bowel Syndrome (IBS) is actually one of the clearest examples of the gut–brain link. A lot of people who have IBS notice that their symptoms flare up particularly when they’re stressed and anxious.
In fact, a lot of research correlates having IBS with depressive/anxiety symptoms.
At The Health Suite Leicester, we help patients break this cycle by addressing both the gut symptoms and the psychological stress response – not treating them as separate issues, but as two sides of the same coin.
Diet and Mood: You Are What You Eat?
Have you ever heard of the adage “you are what you eat”?. And as it turns out, the reasons for this go even deeper than we think. That’s because your microbiome thrives on what you feed it. So if you eat a diet full of processed foods, sugar, and artificial additives, you promote the growth of “bad” bacteria, or bacteria that are less beneficial for you. This, in turn, can increase inflammation and worsen your mood.
The opposite is also true; people who follow a Mediterranean-style diet, which is rich in olive oil, vegetables, fish and legumes, report better mood and lower risk of depression.
Because when your diet contains fibre from whole foods, and polyphenols from fruits, vegetables, nuts and seeds, it helps “good” bacteria flourish. They produce short-chain fatty acids (SCFAs) that have anti-inflammatory effects and may even support healthy brain function.
Probiotics and Mood
Scientists have started exploring what we call “psychobiotics” – these are strains of probiotics that have, in some studies, been found to support mental health.
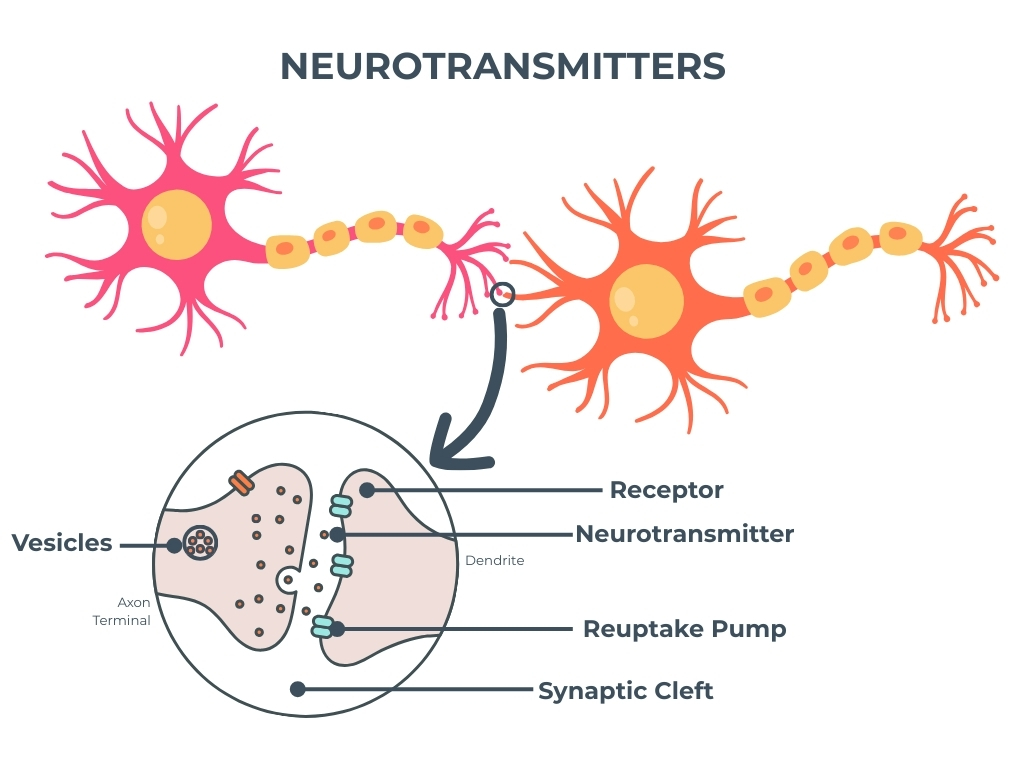
Some probiotic strains also seem to influence the production of neurotransmitters like serotonin and gamma-aminobutyric acid (GABA), which are both critical for reducing anxiety and regulating overall mood.
Production of Neurotransmitter in the Gut
It might sound unbelievable but 90% of serotonin which is often dubbed the “happiness chemical” is produced in the gut.
Our gut bacteria serve a role in the production of these neurotransmitters that affect mood and behaviour. When it’s imbalanced, this neurotransmitter can also be affected, which is a contributor to mood disorders like depression and anxiety.
It goes to show that treating mental health purely at the level of the brain may miss part of the bigger picture. Supporting gut health is often a missing link in restoring balance.
Immune System Regulation and Inflammation
Home to a large portion of the body’s immune cells, the gut and its microbiome help regulate inflammation and maintain balance.
With damage to the gut lining over time, you can develop something we call “leaky gut” or increased intestinal permeability. This is where the intestinal lining becomes more porous than it should be, and therefore allows undigested food particles, toxins, and bacteria to pass into the bloodstream, which triggers various health issues and inflammation.
What’s more, chronic, low-grade inflammation is strongly associated with depression, fatigue and cognitive decline. By improving gut health, we can calm the immune system and, in turn, support more stable mental health.
The Role of the Vagus Nerve
The vagus nerve is central to the gut-brain connection and acts like a communication superhighway; signals travel in both directions: the gut can influence mood via the vagus nerve, and the brain can impact digestion.
Stimulating vagal tone, through practices like deep breathing, meditation, or even certain therapies, can improve both gut health and mental well-being.
Gut–Brain Connection Care at The Health Suite Leicester
At The Health Suite Leicester, our approach is different. We don’t just look at digestion in isolation — we take a personalised, whole-body view of the gut–brain connection, recognising how strongly your gut health influences mood, energy, and overall wellbeing.
Our programmes may include:
- Advanced Gut Microbiome Testing – to uncover bacterial imbalances, digestive issues, and nutrient absorption problems.
- Individualised Nutrition Plans – tailored to encourage beneficial bacteria and support better mood regulation.
- Probiotic and Supplement Strategies – guided by your unique microbiome profile to restore balance and resilience.
- IV Nutrient Therapy – to correct deficiencies quickly when absorption through the gut is compromised.
By combining the best of scientific testing with a holistic philosophy, we create a pathway not only to better digestion but also to improved energy, stronger immunity, and enhanced emotional well-being.
The Bigger Picture
The link between the gut and the brain is a powerful reminder that mental health is not just “in the mind” — it has a biological foundation we can influence. The foods you eat, the balance of your gut microbiome, and even the integrity of your gut lining all send signals to the brain. These signals can affect mood, focus, energy, and overall emotional well-being, showing just how closely your digestive health and mental health are connected.
The Bottom Line
Whilst the relationship between the gut and the brain is a complex one, one thing is clear: when the gut is fed well, the brain can truly thrive. But when there’s a microbiome imbalance or inflammation in our gut, our mental health can suffer in ways we’re not truly cognizant of.
At The Health Suite, we use personalised testing, tailored nutrition, and advanced therapies to help patients optimise the gut–brain connection — supporting not only physical health, but also mental clarity, emotional balance, and long-term resilience.
Take the Next Step
If you’ve been struggling with IBS, anxiety, low mood, or unexplained fatigue, it may be time to look deeper at your gut health.
Book a consultation with our nutritionists or Functional Medicine doctor at The Health Suite Leicester to explore how your microbiome may be affecting your mental health, and discover a personalised plan to restore balance, clarity, and vitality.
Boost your mood and gut health with tailored Nutritional Therapy.