Diverticulitis is a digestive health condition that can vary from mild discomfort to life-altering complications [1]. While the condition is becoming more common globally, [2] research continues to show that with changes in diet and lifestyle, it is possible to manage symptoms, reduce flare-ups, and in some cases prevent progression altogether [3].
Nutrition sits at the centre of this process [1]. With the guidance of a nutritionist, individuals can better understand how food and lifestyle choices impact their digestive health and implement strategies that ease the burden of the disease while promoting long-term gut resilience.
Understanding Diverticulitis as an Inflammatory Condition
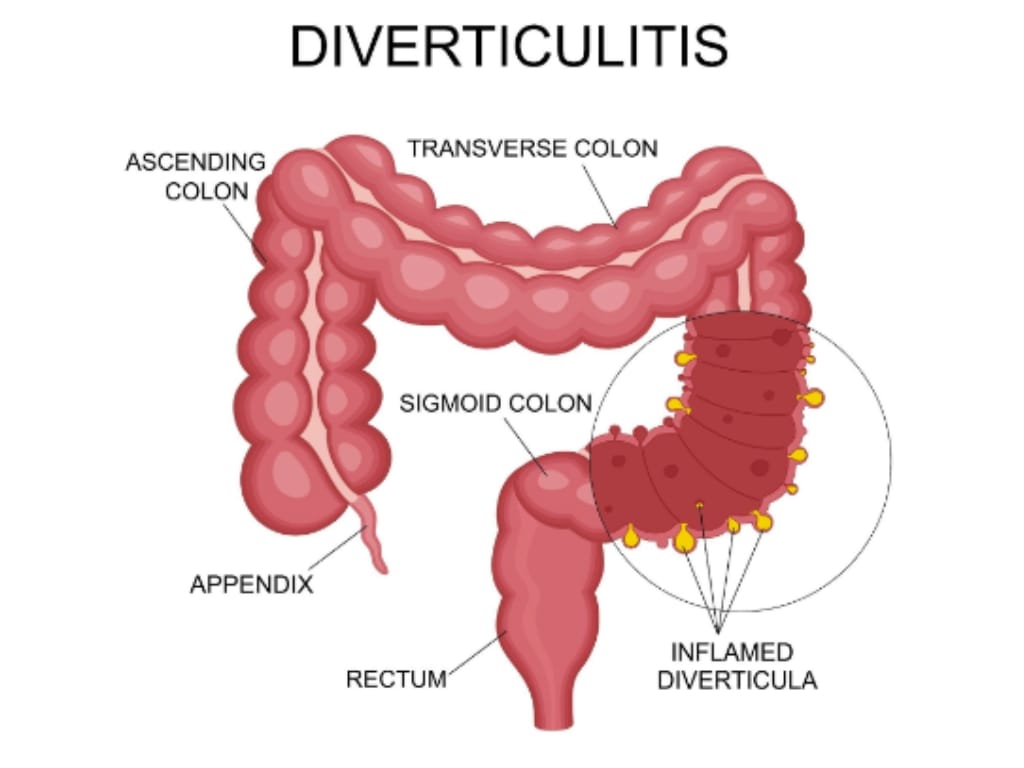
Diverticulitis develops when small bulges or pockets in the lining of the colon, known as diverticula, become inflamed or infected [4]. For many people, these pouches form due to years of increased pressure in the colon, often associated with a low-fibre diet [4]. In some, they remain harmless (diverticulosis), but when infection develops, diverticulitis can follow [5].
Prevalence of the condition rises with age [6]. In the UK, diverticular disease is widespread, affecting between one in three and one in two people at some point in their lifetime [7] – statistics that rise even higher with age, reaching 80% among those over 85 years old. Among those with diverticulosis, about 10-25% will experience diverticulitis during their lifetime [8].
Recent data indicate that diverticulosis is increasingly being diagnosed in younger age groups, with incidence rates rising in part due to modern lifestyle factors, including low-fibre diets and rising obesity [9]. Additionally, lifestyle factors such as smoking and physical inactivity are closely linked to diverticular disease risk, emphasising the multifactorial nature of this condition and the role of comprehensive management strategies [9].
The risk of developing acute diverticulitis among those with diverticulosis is around 10-25% over a lifetime [10], and individuals experiencing complicated diverticulitis can face short-term mortality rates exceeding 8%, with long-term rates climbing to nearly 15% if perforation occurs [11].
Recognising Symptoms and the Importance of Diagnosis
Recognising the symptoms of diverticulitis can be challenging, as early signs often resemble other common conditions like irritable bowel syndrome, appendicitis, or urinary infections [1].
Typically, symptoms include persistent lower left abdominal pain, fever, nausea, vomiting, and changes in bowel habits such as diarrhoea, constipation, or bloating [4]. While mild cases may resolve without intervention or remain undiagnosed, more severe episodes can lead to serious complications, including abscesses, bowel perforation, or peritonitis – conditions that require urgent medical attention [1].
Early and accurate diagnosis is crucial [12]. Healthcare professionals usually perform a physical exam, checking for tenderness or guarding in the lower abdomen [13]. Laboratory tests – such as blood tests for infection markers and stool analysis – help rule out other conditions [1]. Imaging, primarily contrast-enhanced CT scans, is regarded as the gold standard for diagnosing acute diverticulitis and detecting complications like abscesses or perforation [14].
In some cases, endoscopy or colonoscopy may be used after the initial episode to rule out other issues such as bowel cancer, especially in cases with atypical symptoms.1 Timely diagnosis allows prompt treatment, which can prevent the progression to life-threatening complications like peritonitis or bowel obstruction.
Risk factors that increase the likelihood of developing diverticulitis include age, diet, and particularly a low-fibre intake [4] [7]. Obesity further amplifies this risk; for example, men with a BMI ≥30kg/m had a relative risk of 1.78 for diverticulitis and 3.19 for diverticular bleeding, compared to men with a BMI of <21kg/m.15 Research from the US has also shown women who gained 20kg or more had an 80% increased risk compared to those maintaining their weight with loss or gain no greater than 2kg, highlighting the significant impact of weight gain as well as baseline obesity on disease risk [16].
Acknowledging The Nutritionist’s Role in Management
Managing diverticulitis effectively requires a comprehensive approach, and diet plays a foundational role in both preventing flare-ups and supporting recovery [3]. This is where the expertise of a nutritionist becomes invaluable. Nutritionists assess each individual’s unique needs, challenges, and lifestyle, creating personalised dietary plans that not only reduce inflammation but also enhance overall digestive health.
Contrary to previous beliefs that patients with diverticulitis should avoid fibre, current evidence strongly supports the inclusion of a high-fibre diet to manage symptoms and lower the risk of future attacks [17]. A nutritionist guides patients in gradually increasing fibre intake from sources such as fruits, vegetables, whole grains, legumes, and seeds, ensuring gentle and sustained improvements in bowel regularity and colon health.
Studies show that individuals consuming 30g of fibre per day have a 41% reduction in risk compared to persons with a low fibre intake [18]. Furthermore, a high-fibre diet helps soften stools and reduce pressure within the colon, addressing one of the root contributors to diverticular disease. Nutritional analyses also suggest many patients with diverticulitis consume diets high in saturated fat and animal protein but low in magnesium, calcium, zinc, and vitamin E, nutrients essential for intestinal motility and inflammation control. Correcting these deficiencies through diet can be an important part of management.
Hydration is another key focus. Fibre’s effectiveness depends on adequate fluid intake, with nutritionists recommending at least 1.5 to 2 litres of water daily to facilitate optimal stool softness and movement. Additionally, physical activity – such as walking, swimming, or pilates – is encouraged to enhance gut motility and reduce constipation-related complications.
During an acute flare-up, a nutritionist may recommend a temporary low-fibre or clear liquid diet to allow the colon to rest and heal while managing symptoms. As inflammation subsides, they carefully reintroduce fibre-rich foods tailored to tolerance and symptom control, preventing malnutrition and promoting gut microbial balance. Nutritionists also support patients in identifying and avoiding personal trigger foods through food and symptom diaries.
Obesity is a significant modifier of disease severity and recurrence risk. Nutritionists provide crucial support in weight management through sustainable dietary changes and lifestyle coaching, aiming to reduce the increased risk associated with a high BMI. This holistic guidance often integrates stress management techniques, given that stress can exacerbate symptoms by disrupting gut function.
By partnering with a nutritionist, individuals with diverticulitis gain personalised, evidence-based strategies for dietary management and lifestyle changes. The success of this collaborative approach is exemplified by studies that report outpatient treatment as a safe and effective therapeutic approach in up to 90% of patients with uncomplicated diverticulitis [19], with dietary management a consideration in this approach.
Moving From Flare-ups to Long-term Wellness
For many living with diverticulosis or recovering from diverticulitis, the focus naturally shifts from managing acute flare-ups to achieving sustained digestive wellness and preventing recurrence.
Diverticulitis flare-ups typically resolve within two weeks with appropriate treatment, but about 10-35% of people experience another episode after a first [20], highlighting the importance of proactive long-term strategies rather than reactive crisis management. However, early follow-up is recommended to help improve outcomes by allowing timely reassessment and adjustment of care plans, reducing hospital readmissions and preventing progression to complicated disease.
A key aspect of moving toward lasting health is gradually transitioning from symptom-focused care – such as low-fibre or liquid diets during flare-ups – to a balanced, high-fibre diet that supports colon integrity and reduces pressure within the bowel. Research shows that a high-fibre diet can reduce the risk of recurrent diverticulitis and decrease hospitalisations due to diverticular disease [18].
This gradual, evidence-based lifestyle shift can be supported by nutritionists who personalise dietary plans and lifestyle advice, helping patients adapt fibre intake, hydration, and exercise based on tolerance and progression. Through ongoing professional guidance, the journey from frequent acute episodes to long-term stability becomes achievable, empowering individuals to regain energy, reduce complications, and enhance quality of life.
Taking Control of Your Situation With The Health Suite
Receiving a diagnosis of diverticulitis or diverticulosis can be unsettling, but it’s also a powerful moment to take control of your health and set a new course for your future.
At The Health Suite, we believe that a proactive, personalised approach brings the best outcomes – not just in managing current symptoms, but in building long-term digestive wellbeing. Our aim is to empower you, transforming what can feel like a limiting diagnosis into an opportunity for meaningful, positive lifestyle change.
From your first consultation, our experienced nutritionists and multidisciplinary team work closely with you to assess your unique needs, medical history, and lifestyle. We create tailored nutrition plans focused on gradually increasing dietary fibre, optimising hydration, and carefully introducing foods that promote gut health and reduce the risk of recurrence. During flare-ups, your care is adapted to provide short-term symptom relief while building toward sustained improvement in your dietary routines.
Most importantly, we empower you to understand your body’s signals, create sustainable routines, and embrace an active role in your self-care. Evidence shows that consistent dietary and lifestyle changes under expert supervision dramatically lower the risk of diverticulitis recurrence and long-term complications [21], supporting not only gut function but greater energy and quality of life.
With The Health Suite Leicester at your side, taking control becomes not just possible – but achievable, collaborative, and supported every step of the way.
Find out more about our diverticulitis dietary support at The Health Suite and how it could benefit you here:
Manage Diverticulitis with Nutritionist-Led Dietary Guidance
References:
- NHS. Diverticular disease and diverticulitis. Available at: https://www.nhs.uk/conditions/diverticular-disease-and-diverticulitis/
- Neylan CJ, et al. The Epidemiology of Diverticulitis. Clin Colon Rectal Surg. 2024; 4;38(4):241-248
- Piotrowicz G, et al. Managing diverticula: dietary changes for a more comfortable life. Prz Gastroenterol. 2025;20(1):92-101
- NHS Inform. Diverticular disease and diverticulitis. Available at: https://www.nhsinform.scot/illnesses-and-conditions/stomach-liver-and-gastrointestinal-tract/diverticular-disease-and-diverticulitis/
- InformedHealth.org. Diverticular disease and diverticulitis: Learn More – Treating acute diverticulitis. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006
- Hawkins AT, et al. Diverticulitis: An Update From the Age Old Paradigm. Curr Probl Surg. 2020;57(10):100862
- Guts UK. Diverticular Disease. Available at: https://gutscharity.org.uk/advice-and-information/conditions/diverticular-disease/
- Wilkins T, et al. Diagnosis and management of acute diverticulitis. Am Fam Physician. 2013; 87(9), 612-620
- Glass B., Dalia S. Diverticulitis Becoming More Prevalent Amongst Younger Generations: What to Look For? Annals of Medicine and Medical Sciences. 2024; 3, 5-8
- Williams S, et al. Diverticular disease: update on pathophysiology, classification and management. Frontline Gastroenterol. 2023; 27;15(1):50-58
- Papenfuss WA, et al. Clinical outcomes and mortality in complicated diverticulitis: A systematic review and meta-analysis. The Lancet Gastroenterology & Hepatology. 2020; 5(5), 495-507
- NICE. Evidence review for diagnostic tests for acute diverticulitis: Diverticular disease: diagnosis and management. Available from: https://www.ncbi.nlm.nih.gov/books/NBK558084/
- NIDDK. Diagnosis of Diverticular Disease. Available at: https://www.niddk.nih.gov/health-information/digestive-diseases/diverticulosis-diverticulitis/diagnosis
- NICE. Diverticular disease: diagnosis and management. NG147. Available at: https://www.nice.org.uk/guidance/ng147/chapter/rationale-and-impact
- Strate LL, et al. Obesity increases the risks of diverticulitis and diverticular bleeding. Gastroenterology. 2009;136(1):115-122.e1
- Ma W, et al. Association Between Obesity and Weight Change and Risk of Diverticulitis in Women. Gastroenterology. 2018;155(1):58-66.e4
- Peery AF, Sandler RS. Diverticular disease: reconsidering conventional wisdom. Clin Gastroenterol Hepatol. 2013;11(12):1532-7
- Aune D, et al. Dietary fibre intake and the risk of diverticular disease: a systematic review and meta-analysis of prospective studies. Eur J Nutr. 2020;59(2):421-432
- Tursi A. Efficacy, safety, and applicability of outpatient treatment for diverticulitis. Drug Healthc Patient Saf. 2014; 31;6:29-36
- Al Harakeh H, et al. Recurrent Acute Diverticulitis: When to Operate? Inflamm Intest Dis. 2018;3(2):91-99
- Carabotti M, et al. Role of Dietary Habits in the Prevention of Diverticular Disease Complications: A Systematic Review. Nutrients. 2021; 14;13(4):1288.
