Irritable Bowel Syndrome (IBS) is a common, complex chronic disorder of gut-brain interaction that can range from recurrent abdominal pain to mild bloating and discomfort to unpredictable bowel habits (or a combination of these) [1][2]. Although IBS does not cause structural damage to the digestive tract, it can have a life-altering impact on daily life, contributing to anxiety, fatigue, and social withdrawal for many people [1][4][5].
Despite functional gastrointestinal disorders impacting 40% of the global population, and IBS contributing to more than a third of that figure (14.1%) [6], IBS remains underdiagnosed and often misunderstood [2]. However, contemporary research shows that with the right dietary strategies and lifestyle changes – particularly under the guidance of a nutritionist – symptoms can be significantly reduced, helping individuals regain comfort, control, and a broader sense of wellbeing [7][8][9].
At the centre of effective IBS management lies a holistic understanding of how foods, gut-brain interactions, and lifestyle factors contribute to symptom flare-ups. Nutritionists play a pivotal role in helping people navigate these triggers, rebuild gut resilience, and develop routines that align with both their biology and lifestyle.
Understanding IBS as a Functional Disorder
IBS is classified as a functional gastrointestinal disorder, which means the digestive system looks physically normal but functions abnormally [10]. It is characterised by recurrent abdominal pain associated with changes in bowel habits – such as diarrhoea (IBS-D), constipation (IBS-C), or alternating patterns (IBS-M) [11].
Unlike inflammatory conditions such as Crohn’s disease or ulcerative colitis, IBS does not cause visible intestinal inflammation or damage, yet its symptoms can be equally debilitating, often affecting concentration, mood, and quality of life due to their chronic and unpredictable nature [12].
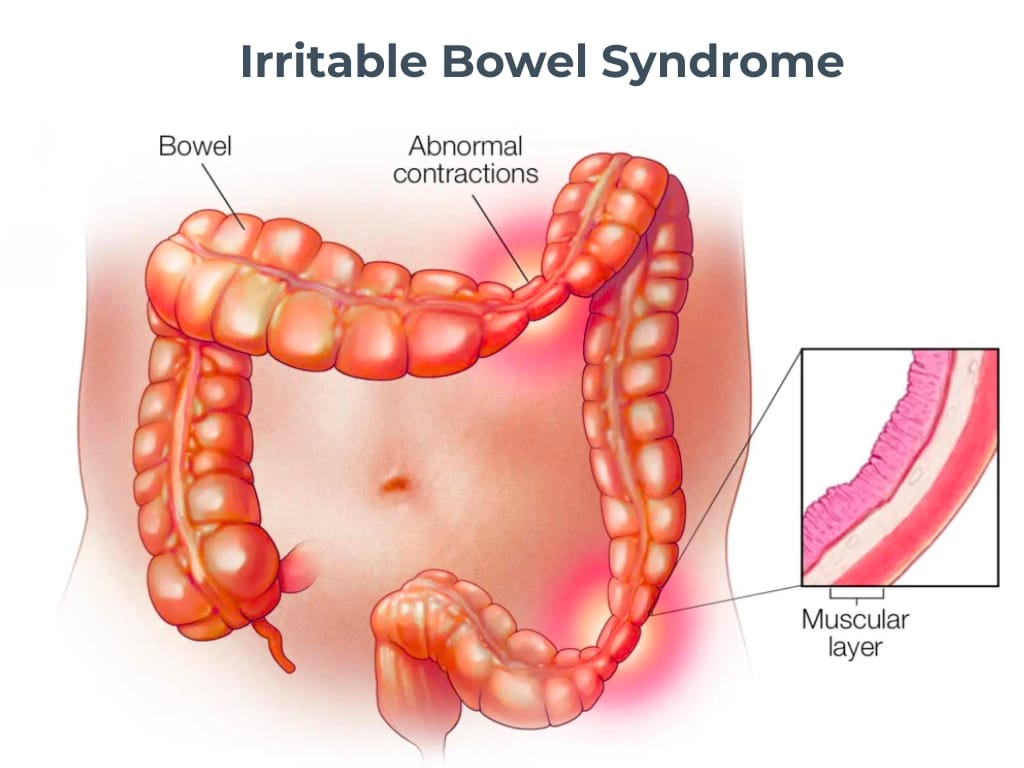
Many researchers now highlight the gut-brain axis as a key factor in IBS [13], suggesting that miscommunication between the central nervous system and the digestive tract can heighten sensitivity, disrupt motility, and trigger symptom flare-ups in response to stress or dietary changes. This can lead to increased gut pain perception (known as visceral hypersensitivity), irregular bowel movements, and changes in gut microbiota composition [13].
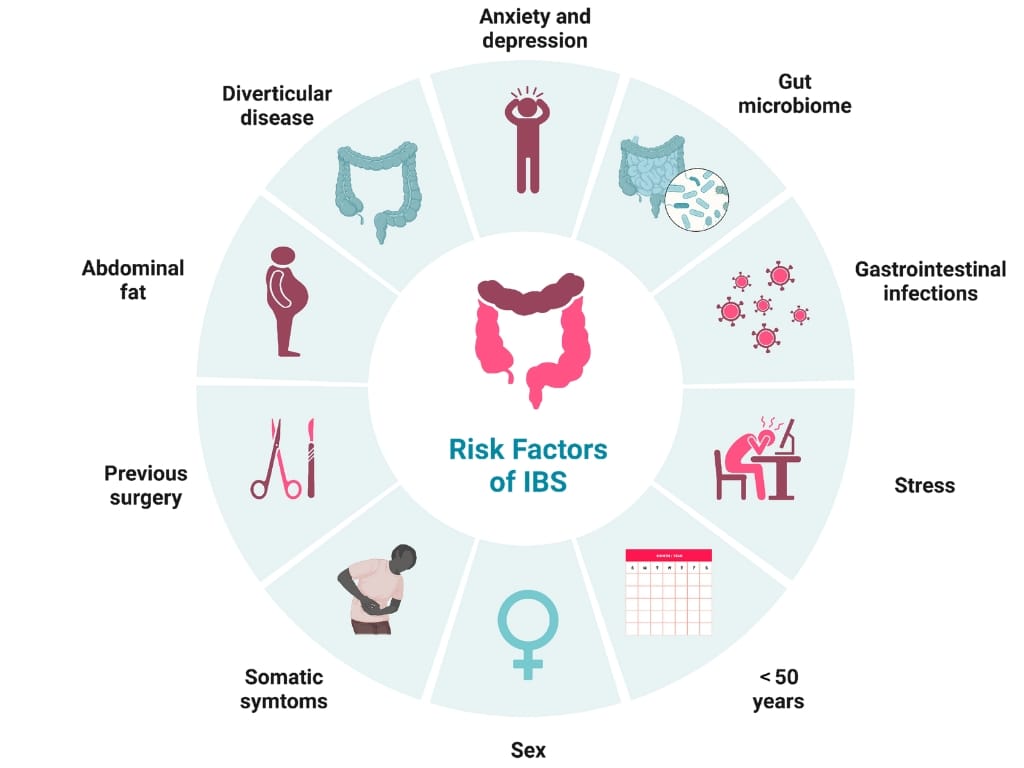
IBS often begins in young adulthood, with women being nearly twice as likely to be affected as men [14]. In the UK, an estimated 13 million people live with IBS, according to NHS data [15], with most cases diagnosed between the ages of 20 and 40 [14]. Severity rates differ in the community, with 31.4% reporting mild IBS, 48.3% reporting moderate IBS, and 20.3% reporting severe IBS [16].
While the exact cause of IBS is not fully understood, lifestyle factors – including stress, disrupted sleep, high-fat diets, and antibiotic use – are all thought to play roles in both onset and exacerbation [17]. That is why, for example, we see ‘Western’ diets, which are characterised by higher consumption of fatty and sugary products, sweetened beverages, snacks and starches, associated with an increased risk of IBS [18].
Recognising Symptoms and Seeking Diagnosis
IBS presents with a wide range of gastrointestinal and systemic symptoms that may fluctuate over time. The most common include abdominal pain or cramping relieved by passing stool, bloating, excessive gas, and alternating episodes of diarrhoea and constipation [1][10]. Some people also experience fatigue, nausea, and the sensation of incomplete bowel movements [4].
Many people find it helpful to track their symptoms and dietary habits to identify potential triggers such as caffeine, fatty foods, or artificial sweeteners. Keeping a food and symptom diary can support both personal awareness and clinical discussions, enabling more targeted management strategies.
Early professional evaluation is essential, not only to confirm IBS but also to rule out other serious gastrointestinal conditions. Diagnosis is largely clinical and based on Rome IV criteria, requiring recurrent abdominal pain for at least one day per week over three months, accompanied by two or more features relating to stool frequency or appearance [6].
However, since there are no definitive diagnostic tests, healthcare professionals often rule out other conditions such as coeliac disease, inflammatory bowel disease, or lactose intolerance.
Testing during this stage may include:
- Blood tests to check for anaemia or inflammation
- Stool analysis to rule out infection or gut inflammation
- Colonoscopy or imaging if red flag symptoms such as bleeding, unexplained weight loss, or persistent vomiting occur [19].
Given IBS can be strongly influenced by stress and emotional factors, with up to 60% of patients reporting increased symptoms during periods of anxiety or life changes [20], there is an evident need for a multidisciplinary approach to care; one that combines nutrition, lifestyle guidance, and psychological support.
The Nutritionist’s Role in IBS Management
Dietary modification can be one of the most effective tools for controlling IBS symptoms, and this is where a nutritionist’s guidance is crucial. They work to identify individual food triggers, correct nutrient imbalances, and restore a balanced gut microbiome while supporting emotional and physical well-being.
For many patients, the low FODMAP diet has transformed symptom management [21]. FODMAPs – fermentable oligo-, di-, monosaccharides and polyols – are short-chain carbohydrates that can cause gas and water retention in the bowel, triggering pain and bloating in sensitive individuals [22]. Under a nutritionist’s supervision, patients first exclude high-FODMAP foods (such as onions, garlic, wheat, beans, and certain fruits), then methodically reintroduce them to identify tolerances. Evidence shows that up to 70% of people with IBS experience improved symptoms on a structured low FODMAP plan [23].
A nutritionist also helps protect against nutritional deficiencies during the elimination phase, ensuring adequate intake of fibre, calcium, and B vitamins. Whole, unprocessed foods are prioritised, with portions of soluble fibre from oats, psyllium, and flaxseed recommended to ease constipation and improve stool consistency [24].
Beyond FODMAP management, nutritionists often address other dietary triggers such as caffeine, alcohol, fatty foods, and artificial sweeteners, which can all worsen gastrointestinal symptoms. Hydration also plays a vital role: drinking 1.5-2 litres of water daily helps regulate bowel movements and counteracts bloating [7].
Stress management techniques, such as mindful eating, breathing exercises, and gut-directed hypnotherapy, have been shown to significantly improve quality of life in IBS patients. By addressing both physiological and psychological components of digestion, nutritionists offer a balanced, evidence-based path to symptom control.
From Flare-Ups to Long-Term Gut Health
While IBS is a chronic condition, symptoms can be greatly minimised through consistent diet and lifestyle changes. Flare-ups are often linked to stress, dietary excess, or infection, but with careful management, many people achieve long-term stability.
In fact, observational case-control studies and randomised, controlled trials generally support the use of a low-FODMAP diet for patients with IBS, as 50% to 80% of patients report some benefits compared to using a regular or habitual diet [25].
Rebalancing the gut microbiota through food diversity, prebiotics, or targeted probiotics may also enhance resilience and reduce sensitivity. Nutritionists use tools such as food diaries and symptom scoring to pinpoint personal triggers, gradually enabling independence in managing flare-ups.
Building on this foundation, other lifestyle adjustments can play a major role in preventing future IBS flare-ups. Eating smaller, more frequent meals and steering clear of high-fat, spicy, and processed foods can help reduce digestive discomfort, while drinking plenty of water and getting adequate fibre from well-tolerated sources improves regularity.
Beyond food, establishing a routine that supports gut regularity – including sufficient sleep, physical activity, and mindful eating – is key to reducing recurrence. Consistent stress management through mindfulness practices, exercise, and relaxation techniques has also been shown to calm the gut-brain axis and decrease symptom severity.
Rather than focusing solely on short-term relief, modern IBS management emphasises rebuilding a healthy gut-brain connection and nurturing the microbiome to support long-term digestive comfort.
Taking Control of Your IBS With The Health Suite
A diagnosis of IBS can feel frustrating and confusing – but it is also an important opportunity to take control and reshape your digestive health for the better.
At The Health Suite, we take a personalised approach to IBS management that begins with understanding you: your diet, habits, stress factors, and goals. Our approach extends beyond symptom management to nurture a deeper understanding of your body’s unique responses.
Through regular check-ins, progress tracking, and lifestyle coaching, we help you identify patterns and make confident, informed choices. Whether it’s navigating dining out, travelling, or managing stress during busy periods, our team provides sustainable tools that fit your real life.
By integrating nutrition, movement, and mindfulness, The Health Suite empowers you to build a strong, lasting foundation for digestive wellness and overall vitality, with a focus on three key areas:
- Symptom relief through specialist dietary intervention, including customised low FODMAP strategies
- Gut restoration through balanced fibre intake, probiotic support, and gradual reintroduction of tolerated foods
- Long-term resilience, helping you build routines around hydration, movement, and mindful eating.
With compassionate support and evidence-based strategies, living well with IBS is not only possible but completely achievable. Together, we’ll help you move from reactive management to proactive control – empowering you to enjoy everyday life with confidence and comfort.
Find out more about our nutritionist-led IBS support at The Health Suite and how it could benefit you here: Nutritional Therapy at The Health Suite Leicester.
Explore our nutritionist-led IBS support at The Health Suite Leicester.
