Polycystic Ovary Syndrome (PCOS) is a complex hormonal condition that affects the ovaries, leading to a range of health challenges that negatively impact women’s health [1].
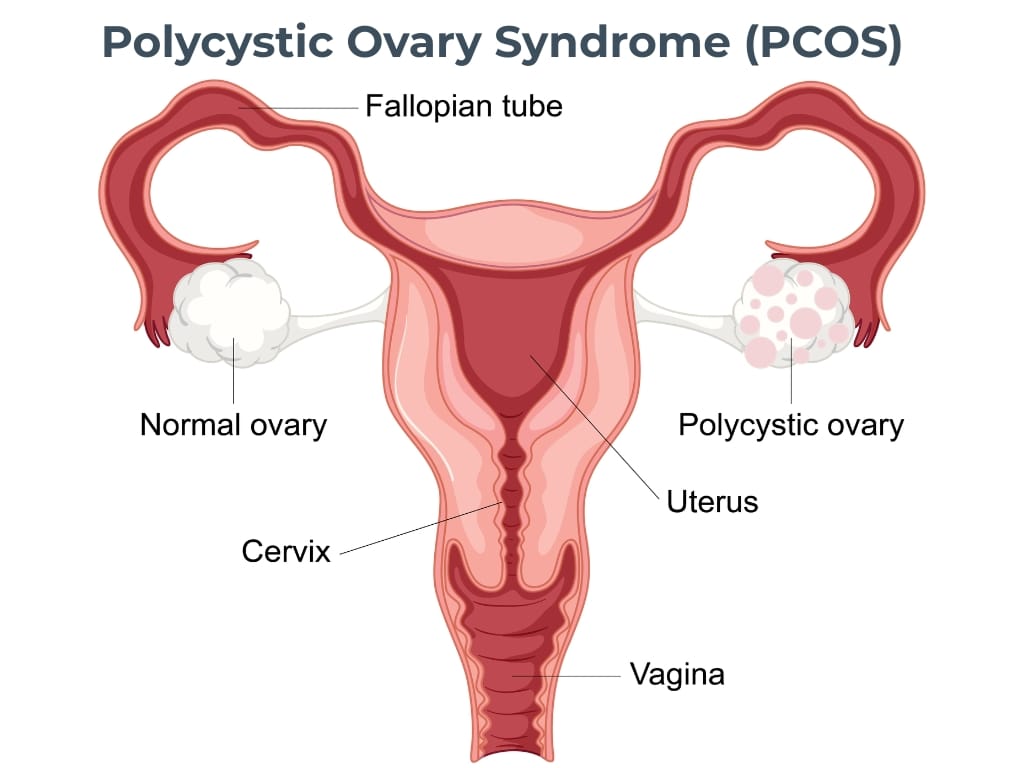
PCOS is not a single condition but rather a spectrum of interrelated symptoms and risks that can significantly impact physical and emotional well-being. It is characterised by the presence of multiple small cysts on the ovaries, hormonal imbalances including excess androgen levels, metabolic disturbances such as insulin resistance, and irregular periods [2].
Estimates suggest that approximately 10% of women in the UK live with PCOS, [2] though prevalence rates can vary between 6% and 13% of reproductive-aged women depending on diagnostic criteria and populations studied [1]. Research shows that up to 70% of women with PCOS may remain undiagnosed [1], often because symptoms can be subtle, overlap with other conditions, or are dismissed as normal hormonal fluctuations.
PCOS affects women across all ethnicities and backgrounds, though the expression of symptoms and metabolic risks can differ between groups [3]. Its status as one of the most common reproductive endocrine disorders is the marker of one of the most significant public health challenges – one compounded by its association with increased risks of diabetes, cardiovascular disease, endometrial cancer, and mental health conditions [1].
Understanding the Biology of PCOS
At a biological level, PCOS reflects a disruption in the normal functioning of the ovaries, driven primarily by hormonal imbalances and abnormal ovarian structure [4]. One of the defining features of PCOS is the presence of multiple small cysts – technically referred to as immature follicles – clustered around the periphery of the ovaries. These polycystic ovaries result from a failure of the follicles to mature and release eggs during the menstrual cycle, leading to irregular or absent ovulation [2,5].
Central to this process is an excess production of androgens, sex hormones more commonly associated with male traits but naturally present in all women at lower levels [1,5].
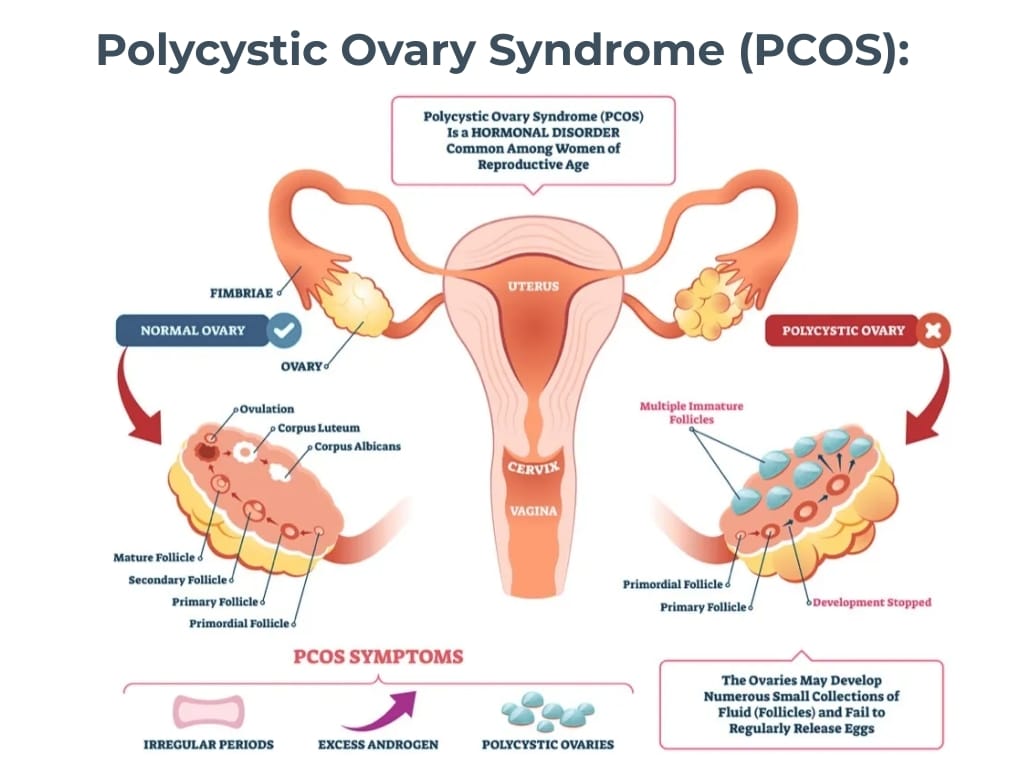
In PCOS, the ovaries (and sometimes the adrenal glands) release higher-than-normal amounts of androgens, which disrupt the delicate hormonal feedback loops that regulate ovulation [1,5]. Elevated androgen levels can also contribute to classic symptoms such as excess hair growth, acne, and scalp hair thinning [6].
Insulin resistance often plays a critical role in PCOS’s pathophysiology [2]. When the body’s cells become less responsive to insulin, the pancreas compensates by producing more, resulting in hyperinsulinemia. This excess insulin stimulates the ovaries to increase production of hormones like testosterone and androgen, further exacerbating the hormonal imbalance [2,7]. Moreover, insulin resistance contributes to weight gain and increases the risk of developing type 2 diabetes – common concerns for many women with PCOS [2,8].
This complex hormonal crosstalk not only affects reproductive health but also influences metabolism, inflammation, and cardiovascular risk factors [8]. As a result, PCOS is increasingly understood as a multisystem condition requiring holistic management beyond fertility concerns.
Recognising How PCOS Manifests in Daily Life
PCOS is notorious for its wide-ranging and often unpredictable symptoms, which can make daily life a balancing act for the women it affects. While some may primarily experience irregular menstrual cycles or difficulty conceiving, others might grapple with persistent acne, unwanted hair growth, or the physical and emotional challenges of weight management [2,6,8]. The condition rarely presents the same way twice, contributing to feelings of frustration and uncertainty.
One of the most immediate and disruptive symptoms is menstrual irregularity. Cycles may be infrequent, prolonged, or absent, complicating family planning and causing distress [2]. For many, this unpredictability can be a constant reminder of underlying hormonal upheaval.
Alongside reproductive challenges, PCOS frequently causes skin issues such as acne and oily skin, often resistant to conventional treatments, and hirsutism – the growth of coarse, dark hair in facial and body areas where it is typically minimal or absent [6].
Individuals with PCOS experience hirsutism, far above the 5-10% prevalence in the general female population [9], highlighting how visible androgen-related symptoms affect many women. These visible signs can profoundly affect self-esteem and social confidence.
Weight gain, particularly around the abdomen, is another common concern. Many women with PCOS find it challenging to lose weight despite dietary efforts and exercise, due in part to the metabolic effects of insulin resistance [2,8]. This struggle adds a layer of complexity to symptom management and can fuel cycles of frustration or emotional distress.
The emotional impact of PCOS should not be underestimated. Rates of anxiety and depression are significantly higher among women with PCOS compared to the general public, influenced by hormonal changes, body image issues, and the stress of chronic condition management.10 The ‘invisible’ burden of PCOS – fatigue, brain fog, and mood instability – often goes unrecognised but further diminishes quality of life and day-to-day functioning. Sadly, the prevalence of anxiety among women with PCOS ranges between 28% and 39%, while depression affects 11% to 25%, rates much higher than in women without the condition [11].
Attempting to Manage the Effects of PCOS
Women living with PCOS often find themselves navigating a complex landscape of self-care strategies, medical advice, and sometimes conflicting information. Due to the condition’s varied symptoms and underlying causes, there is no universal cure or simple fix, which can make management feel overwhelming and frustrating.
Many first turn to lifestyle modifications, knowing that diet and exercise are foundational to hormonal and metabolic health. Adjusting to a balanced diet that emphasises low-glycemic index foods – such as whole grains, lean proteins, healthy fats, and abundant vegetables – can support insulin sensitivity and weight management [12].
Regular physical activity, including a mix of cardiovascular workouts and strength training, often complements nutritional efforts by improving metabolism, mood, and overall well-being. However, these changes require sustained effort and often deliver gradual improvements, which can test patience and motivation. In fact, while these combined lifestyle changes can significantly improve reproductive function and metabolic markers, studies indicate that sustaining such changes challenges many; research shows up to 50% dropout rates in weight loss trials among women with PCOS, compared to approximately 31% in the general population [13].
Weight management, in particular, is a challenge. Due to insulin resistance and hormonal imbalances, many women with PCOS struggle to lose weight despite commitment to healthy eating and exercise. This can cause discouragement and cyclical weight gain, increasing both physical and emotional burden. Fad diets and quick-fix supplements are sometimes trialled out of frustration, yet these often yield limited or temporary results and can further complicate metabolism.
Medical treatments may also be pursued alongside lifestyle efforts. Hormonal contraceptives are commonly prescribed to regulate menstrual cycles and reduce androgen-related symptoms, while insulin-sensitising medications like metformin aim to improve metabolic profiles [14]. Some women explore fertility treatments when conception is desired [14]. Yet for many, medications address symptoms rather than the root causes or broader health impacts of PCOS.
Supplements such as inositol, vitamin D, and omega-3 fatty acids draw interest for their potential to modulate insulin resistance and inflammation, but their efficacy varies individually and should be guided by healthcare professionals. Meta-analyses suggest inositol, in particular, may improve insulin sensitivity, hormonal profiles, and menstrual regularity, positioning it as a promising adjunct in PCOS management [15]. Still, responses vary, and supplement use is most effective when guided by healthcare professionals within a comprehensive care plan.
Despite the toolbox of strategies, many women report feeling lost navigating their options – uncertain which interventions will help, how to tailor them, and how to sustain progress. This gap highlights the importance of personalised, evidence-based support embedded within a broader healthcare framework.
Adopting a Personalised Approach to PCOS with The Health Suite
At The Health Suite Leicester, managing PCOS means taking a complete and tailored approach that goes beyond treating individual symptoms. We recognise that every woman’s experience of PCOS is unique, which is why we work to understand the whole picture from the very beginning.
Our service includes access to comprehensive private blood tests that assess key hormones such as testosterone, luteinising hormones, and follicle-stimulating hormones, alongside markers like glucose, insulin, and cholesterol. These accurate diagnostics provide essential insights into hormone balance, ovulation patterns, and metabolic health, helping us to identify underlying drivers of PCOS and guide the most effective treatment pathway.
Importantly, these tests are never offered in isolation. We combine results with careful clinical assessment, an understanding of lifestyle factors, and, when appropriate, additional investigations such as ultrasound. This evidence-based, holistic process ensures clarity, avoids fragmented care, and allows patients to feel confident in the decisions being made about their health.
From here, our multidisciplinary team develops personalised care plans that may include nutritional support to improve insulin sensitivity, medical oversight for tailored treatment options, and access to private GPs, endocrinologists, and mental health professionals when needed. This integrated model ensures every aspect of PCOS is addressed, whether that means improving menstrual regularity, supporting fertility, managing weight, or tackling related concerns such as skin and mood changes.
Ongoing follow-up is central to our approach. Through regular check-ins, we review progress, adapt strategies, and provide motivation at each stage of what can often be a challenging journey.
By combining clinical expertise, cutting-edge diagnostics, and compassionate care, The Health Suite Leicester offers women with PCOS both clarity and a practical pathway towards improved health and renewed quality of life.
Find out more about our PCOS support and diagnosis at The Health Suite and how it could benefit you here: PCOS Blood Tests in Leicester
Nutritional therapy at The Health Suite Leicester is designed to support individuals in achieving their health and wellness goals through personalised dietary guidance.
PCOS is a hormonal disorder common among women of reproductive age. It is characterized by irregular menstrual cycles, excess androgen levels (male hormones), and polycystic ovaries, which contain numerous small cysts.
Common symptoms include irregular or missed periods, excessive hair growth (hirsutism), acne, weight gain, thinning hair on the scalp, and difficulty getting pregnant. Some women may also experience dark patches of skin or mood changes.
The exact cause of PCOS is not fully understood, but it is believed to involve a combination of genetic, hormonal, and environmental factors. Insulin resistance is also a common factor in many women with PCOS.
Diagnosis typically involves a combination of medical history, physical examination, blood tests to check hormone levels, and imaging tests like an ultrasound to look for cysts on the ovaries.
Women with PCOS have a higher risk of developing various health issues, including type 2 diabetes, high blood pressure, heart disease, endometrial cancer, and infertility.
While there is no cure for PCOS, symptoms can be managed through lifestyle changes, such as diet and exercise, and medications like hormonal birth control, anti-androgens, and insulin sensitizers.
Adopting a balanced diet low in refined carbohydrates and sugars, engaging in regular physical activity, maintaining a healthy weight, and managing stress can significantly help alleviate symptoms.
Yes, PCOS can run in families, suggesting a genetic component. If a close relative has PCOS, the likelihood of developing the condition may increase.
Yes, many women with PCOS can conceive, although they may face challenges due to irregular ovulation. Treatments like fertility medications can help stimulate ovulation.
Women with PCOS are at an increased risk for mental health issues, such as anxiety and depression, due to the physical symptoms and challenges associated with the condition. Seeking support from mental health professionals can be beneficial.
References:
- World Health Organisation. Polycystic ovary syndrome. Available at: https://www.who.int/news-room/fact-sheets/detail/polycystic-ovary-syndrome
- NHS. Overview. Polycystic Ovary Syndrome. Available at: https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/
- Vanhise K, et al. Racial and ethnic disparities in polycystic ovary syndrome. Fertility and Sterility. 2023; 119(3); 348-354
- Harada, M. Pathophysiology of polycystic ovary syndrome revisited: Current understanding and perspectives regarding future research. Reprod Med Biol. 2022; 8;21(1):e12487
- Healthline. Polycystic Ovary Syndrome (PCOS): Symptoms, Causes, and Treatment. Available at: https://www.healthline.com/health/polycystic-ovary-disease
- Sharma A and Welt C.K. Practical Approach to Hyperandrogenism in Women. Med Clin North Am. 2022; 8;105(6):1099–1116
- NHS. Causes. Polycystic ovary syndrome. Available at: https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/causes/
- CDC. Diabetes and Polycystic Ovary Syndrome (PCOS). Available at: https://www.cdc.gov/diabetes/risk-factors/pcos-polycystic-ovary-syndrome.html
- Mihailidis J, et al. Endocrine evaluation of hirsutism. International Journal of Women’s Dermatology. 2017; 3;1: 6-10
- Dybciak P, et al. Anxiety and Depression in Women with Polycystic Ovary Syndrome. Medicina (Kaunas). 2022; 16;58(7): 942
- Dewani D, et al. The Invisible Struggle: The Psychosocial Aspects of Polycystic Ovary Syndrome. Cureus. 2023; 30;15(12):e51321
- The Association of UK Dieticians. Polycystic Ovary Syndrome (PCOS) and diet. Available at: https://www.bda.uk.com/resource/polycystic-ovary-syndrome-pcos-diet.html#:~:text=Choose%20low%20GI%20carbohydrates%20and,wholegrains%20have%20a%20low%20GI.
- Shagguan F, et al. Effectiveness and acceptability of different lifestyle interventions for women with polycystic ovary syndrome: protocol for a systematic review and network meta-analysis. BMJ Open. 2024;14: e084815
- NHS. Treatment. Polycystic ovary syndrome. Available at:https://www.nhs.uk/conditions/polycystic-ovary-syndrome-pcos/treatment/
- Unfer V, et al. Myo-inositol effects in women with PCOS: a meta-analysis of randomized controlled trials. Endocr Connect. 2017; 20;6(8): 647-658
