Diabetes has become one of the defining health challenges of our time. Worldwide, the numbers are staggering.
According to the World Health Organisation (WHO), in 2022, 830 million individuals were living with diabetes across the globe, and type 2 diabetes accounts for 95% of these cases [1]. An estimated 1.6 million deaths each year are directly attributed to the disease, while millions more suffer long-term complications that profoundly affect quality of life [1].
Yet perhaps the hidden danger lies in prediabetes. By 2030, it is estimated that over 470 million people around the globe will display characteristics suggesting that they may be predisposed to type 2 diabetes [2]. For many, this can be a slow creep that doesn’t dawn until prediabetes diagnosis.
This diagnosis may feel daunting, but more than anything else, it is an opportunity. With the right steps, prediabetes can be reversed, and even type 2 diabetes can often be brought under control or put into remission.
Central to this process is nutritional therapy – an area where, time and again, we see that personalised dietary intervention and lifestyle changes transform lives.
Understanding Prediabetes and Type 2 Diabetes
To understand how nutrition can help, it is first important to understand the conditions themselves. Prediabetes is a high-risk early stage state – a warning signal that blood sugar levels are raised but not yet high enough to qualify as type 2 diabetes [2]. This is sometimes described as a grey zone, a place of heightened risk but also remarkable potential. Research shows that 5-10% of people per year with prediabetes will progress to diabetes,[2] but if addressed swiftly, the body often has the ability to restore blood sugar regulation back to normal.
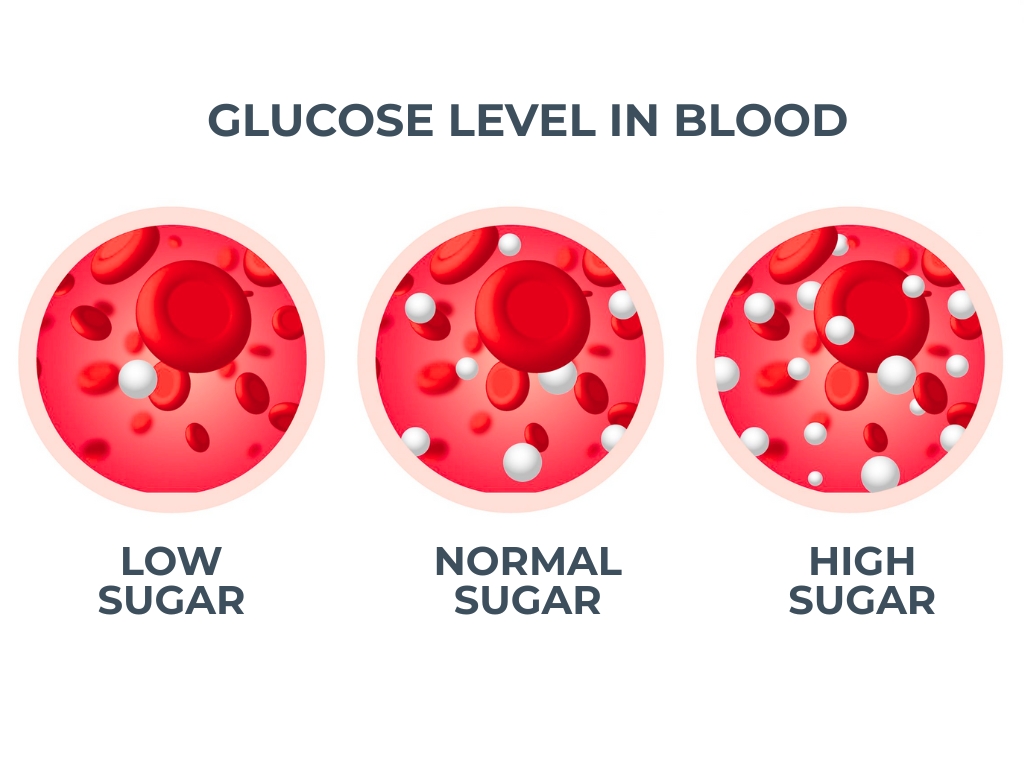
Type 2 diabetes, by contrast, is a chronic condition resulting from insulin resistance [3]. Insulin is the hormone produced by the pancreas that enables glucose – the body’s primary fuel source – to move from the bloodstream into the cells where it can be used for energy [4]. Over time, many people either produce insufficient insulin or their cells become resistant to its action. The result is persistently elevated blood sugar levels, which, if unmanaged, can cause damage to the blood vessels, eyes, kidneys, nerves, and heart [5]. This is why diabetes is considered not only a metabolic condition but also a cardiovascular and systemic disease.
Risk factors are multiple and well-established:
- You are up to x6 more likely to get type 2 diabetes if you have a parent, brother, sister or child with diabetes.
- You are more at risk of type 2 diabetes as you get older.
- You’re more at risk if you’ve ever had high blood pressure.
- You are more at risk if you have a high waist measurement or if you are living with obesity/overweight.
- You are up to x4 more likely to be diagnosed with type 2 diabetes if you are of South Asian, African-Caribbean or Black African descent.
- And type 2 diabetes is also slightly more common in men than in women [6].
Yet there are people who develop the condition without fitting neatly into any of these categories, which speaks to the complex interplay of lifestyle, genetics, and environment.
Recognising Symptoms and the Importance of Diagnosis
Prediabetes can occur without any noticeable symptoms, which makes it particularly dangerous. Many people discover it only through routine blood work [7]. Type 2 diabetes, meanwhile, often announces itself with a set of recognisable signs – thirst, excessive urination, blurred vision, and fatigue among them [8].
The key lies in testing. A result between 5.6-6.9 mmol/L on the fasting plasma glucose tests may indicate there is impaired function, a sign of prediabetes. Over 7.0 mmol/L, and the WHO aligns this to a diabetes diagnosis [9]. Then there is the HbA1c test, which provides a picture of average blood sugar over the past two to three months. If your HbA1c levels are between 42 mmol/mol (6.0%) and 47 mmol/mol (6.4%), you are at risk of developing type 2 diabetes, while 48 mmol/mol (6.5%) or higher is consistent with a diagnosis of diabetes [7]. An oral glucose tolerance test can be used too, with 7.8-11.0 mmol/L recognised as consistent with prediabetes, and 11.1 mmol/L or above confirming diabetes [10].
But this is not just about numbers. Diagnosis represents a critical fork in the road. Left untreated, prediabetes often progresses; around one in four people will develop type 2 diabetes within five years unless they change their lifestyle [11]. On the other hand, those who intervene early can halt the journey entirely, returning blood sugar to safe levels and seeing the markers used to diagnose drop to normal levels.
Acknowledging The Nutritionist’s Role in Management
Managing and potentially reversing prediabetes and type 2 diabetes requires a multifaceted approach, and this is where the support of an experienced nutritionist can be life-changing. A nutritionist does more than create a meal plan. They help you make sense of your body’s signals and the science behind the condition, translating abstract concepts into everyday actions. Education is as crucial as the dietary changes themselves.
One of the most powerful tools in this journey is self-monitoring of blood glucose [12]. Patients are often given devices to track blood sugar, but without proper interpretation, the numbers can be confusing. A nutritionist works through the patterns with you, showing how a particular meal, a stressful day at work, or a bout of exercise influences your readings. Suddenly, the condition can start to feel less mysterious and more manageable.
Dietary changes, of course, sit at the heart of management. Contrary to popular belief, this is not about deprivation but about balance – ensuring that meals contain adequate fibre, lean sources of protein, healthy unsaturated fats, and controlled amounts of complex carbohydrates [13] It is about shifting away from processed foods, sugar-laden snacks, and erratic eating habits towards a consistent, nourishing rhythm that maintains stable energy levels throughout the day [13] Food becomes medicine, but medicine that is enjoyable, flavourful, and sustainable.
Exercise is another cornerstone. Far from being an optional extra, physical activity directly improves insulin sensitivity, meaning the body uses insulin more effectively. For example, structured exercise training has been found to reduce HbA1c by 67% among diabetes patients and improve β-cell function and insulin sensitivity among high-risk patients [14]. And more broadly, a range of physical activities and intensities have been associated with 20% to 30% diabetes risk reduction, especially among high-risk individuals [14].
Moving Toward Better Management
For individuals already diagnosed with type 2 diabetes, the conversation shifts toward management and, increasingly, the potential for remission. While type 2 diabetes is chronic, remission has been demonstrated in growing numbers of patients through structured dietary and lifestyle changes.
The key lies in reducing the burden of excess fat stored in the liver and pancreas – changes that help restore insulin production and sensitivity. In clinical studies, substantial portions of people who lost significant amounts of weight, maintained it, and adhered to carefully planned diets were able to reduce their blood sugar to non-diabetic levels without medication.
This does not mean everyone can or will achieve remission, but it highlights the remarkable impact of targeted lifestyle modifications under professional supervision. Nutrition is a key lever through which the greatest changes can be made. Together with exercise and medical oversight, it can change how we view prediabetes and type 2 diabetes.
Taking Control of Your Situation With The Health Suite
There is no denying that prediabetes and type 2 diabetes present real challenges, both individually and socially. The rising prevalence globally places immense strain on healthcare systems, but on a personal level, the diagnosis can feel like a burden that alters the way you view your body and your future. With the right guidance, the story does not have to feel like this; it does not have to end in decline.
That’s why at The Health Suite Leicester, our philosophy is that no one should face these conditions alone. Support is long-term, designed not only to introduce changes but also to sustain them. Life is not static – holidays, stress, illness, and milestones all bring disruption – and having consistent professional guidance ensures that progress is not lost when circumstances change.
Another distinctive aspect of our approach is integration. You do not just see a nutritionist in isolation. Instead, you become part of a multidisciplinary system that can bring together private GPs, diagnostic blood testing, food sensitivity assessments, and exercise support in one coordinated framework. In some cases, treatments such as weight loss injections may form part of the strategy, prescribed and monitored by our clinical team. This holistic model strengthens the nutritional foundation, ensuring you are not just told what to do but given every tool to succeed.
Working with a nutritionist transforms diabetes management from a reactive process into a proactive one. It gives you the knowledge to understand your body, the tools to adapt to life’s demands, and the support to keep going when motivation wanes. It makes the difference between living at the mercy of fluctuating blood sugars and taking ownership of your health.
At The Health Suite Leicester, our goal is always to meet people where they are and guide them towards where they want to be. Whether you are at the stage of prediabetes with the hope of reversal, or managing type 2 diabetes and seeking remission or stability, our integrated nutritional therapy provides the foundation.
With expert advice and compassionate support, it is possible to move not just towards better numbers on a blood test, but towards greater energy, resilience, and quality of life.
Find out more about our prediabetes and diabetes support at The Health Suite and how it could benefit you here:
Nutritionist-Led Plans to Support Blood Sugar and Diabetes Health
References:
- World Health Organisation. Diabetes. Available at: https://www.who.int/news-room/fact-sheets/detail/diabetes
- Tabák A.G, et al. Prediabetes: a high-risk state for diabetes development. The Lancet. 2012; 379, 9833: 2279-2290
- CDC. About Insulin Resistance and Type 2 Diabetes. Available at: https://www.cdc.gov/diabetes/about/insulin-resistance-type-2-diabetes.html
- NHS Inform. Type 2 diabetes. Available at: https://www.nhsinform.scot/illnesses-and-conditions/diabetes/type-2-diabetes/
- World Health Organisation. Diabetes. Available at: https://www.who.int/health-topics/diabetes#tab=tab_1
- Diabetes UK. Diabetes Risk Factors. Available at: https://www.diabetes.org.uk/about-diabetes/type-2-diabetes/diabetes-risk-factors
- Diabetes UK. Prediabetes symptoms and risk reduction. Available at: https://www.diabetes.org.uk/about-diabetes/type-2-diabetes/prediabetes#:~:text=What%20is%20prediabetes?,than%2Dnormal%20blood%20sugars%20are:
- NHS. Symptoms of type 2 diabetes and how it’s diagnosed. Available at: https://www.nhs.uk/conditions/type-2-diabetes/symptoms/
- Diabetes.co.uk. Fasting Plasma Glucose Test. Available at: https://www.diabetes.co.uk/fasting-plasma-glucose-test.html
- Mayo Clinic. Prediabetes. Diagnosis. Available at: https://www.mayoclinic.org/diseases-conditions/prediabetes/diagnosis-treatment/drc-20355284
- Prakoso D. A, et al. Family Involvement to Stop the Conversion of Prediabetes to Diabetes. Korean J Fam Med. 2023; 14;44(6):303-310
- Diabetes UK. self-monitoring of blood glucose levels for adults with type 2 diabetes (march 2017). Available at: https://www.diabetes.org.uk/about-us/about-the-charity/our-strategy/position-statements/self-monitoring-of-blood-glucose-levels-for-adults-with-type-2-diabetes
- NHS. University Hospitals Sussex. Food Fact: Dietary Advice for Pre Diabetes. Available at: https://www.uhsussex.nhs.uk/resources/food-fact-dietary-advice-for-pre-diabetes/#:~:text=or%20stop%20smoking.-,Manage%20your%20weight,pasta
- Galaviz, K. I, et al. Lifestyle and the Prevention of Type 2 Diabetes: A Status Report. Am J Lifestyle Med. 2015; 24;12(1):4-20
