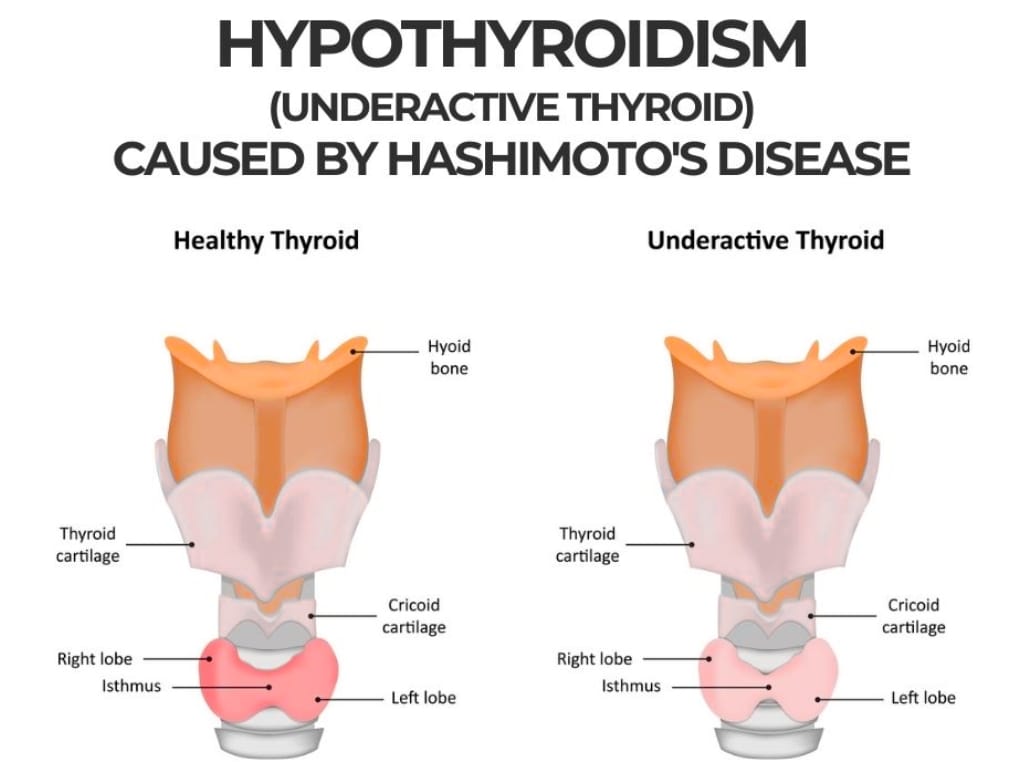
Hashimoto’s thyroiditis and underactive thyroid, often termed hypothyroidism, represent intertwined conditions with significant global impact [1][2]. Both are linked to impaired thyroid gland activity, which disrupts the body’s production of key hormones that regulate metabolism, energy, and growth [1][2].
While hypothyroidism describes the outcome – an underactive thyroid [3]– Hashimoto’s thyroiditis refers to one of its primary causes [4]. In Hashimoto’s thyroiditis, the immune system mistakenly attacks the thyroid tissue, leading to chronic inflammation and a gradual decline in hormone production. Over time, this autoimmune process often results in permanent hypothyroidism [5].
Globally, Hashimoto’s thyroiditis is thought to affect around 7.5% of the population, [2] though prevalence varies widely by region and socioeconomic status. Hypothyroidism, meanwhile, is even more widespread, encompassing both autoimmune and non-autoimmune causes such as iodine deficiency, medication use, or thyroid surgery [1].
Many people with Hashimoto’s thyroiditis or an underactive thyroid face years of unexplained fatigue, weight changes, and low mood before receiving a diagnosis. Even after starting treatment, it is common to feel that some symptoms linger or fluctuate. Increasingly, people are recognising that understanding their body, daily routines, and overall wellbeing plays a big part in feeling their best.
Understanding Hashimoto’s Thyroiditis and Hypothyroidism
Hashimoto’s thyroiditis and hypothyroidism exert much of their impact through the underproduction of thyroid hormones [3],[5]. Still, it is the way they disturb core physiological functions that often leads individuals to seek medical help.
The thyroid gland, located at the base of the neck, plays a pivotal role in maintaining metabolic harmony [6]. It releases hormones such as thyroxine (T4) and triiodothyronine (T3), which regulate cellular metabolism, growth, temperature, and energy levels throughout the body [6].
As production of thyroid hormones declines, a cascade of symptoms and health risks starts to unfold. For some, the changes are subtle at first. For others, symptoms develop gradually over months or even years, making them easy to overlook until they significantly affect day-to-day life.
Recognising the Symptoms of Hashimoto’s Thyroiditis and Hypothyroidism
Early-stage symptoms are frequently subtle or even absent, with many individuals unaware of the underlying dysfunction. Over time, however, the body’s systems begin to respond to the low levels of circulating thyroid hormones.
Fatigue becomes an ever-present companion, unresponsive to rest or lifestyle modification [7]. Individuals also may notice unexplained weight gain, a persistent chill even in warm environments, and pronounced dry skin [8]. Hair loss, brittle nails, and noticeable puffiness – particularly around the face and eyes – may develop as the hormonal imbalance progresses [8][9].
Gastrointestinal disturbances, such as constipation and indigestion, are common, as the slowing of metabolism affects every organ system [10]. Muscles and joints may ache or become weak [8], and the heartbeat slows – sometimes to an extent that disrupts normal cardiac function [3]. Cognitive changes – sometimes termed ‘brain fog’ – are also frequent, ranging from forgetfulness and poor concentration to outright depression or anxiety [11].
Chronic inflammation caused by Hashimoto’s thyroiditis, in particular, has a wide-ranging effect – not only reducing thyroid hormone output but also increasing overall susceptibility to other autoimmune diseases. These may include vitiligo, rheumatoid arthritis, type 1 diabetes, Addison’s disease, pernicious anaemia, and multiple sclerosis, highlighting the interconnectedness of immune dysfunction [12]-[17].
For women specifically, menstrual cycles may become irregular or abnormally heavy, while fertility can be impaired [8][18]. And in children and adolescents, slowed growth and delayed puberty may signal an underlying thyroid condition [19].
Complications related to untreated hypothyroidism are serious and include high cholesterol, elevated cardiovascular risk, heart failure, myxedema (a rare, life-threatening state), [3][20] and, particularly in pregnancy, risks to both mother and child. Symptoms must be taken seriously and addressed proactively [21].
Making Nutrition Part of Management
Today, a nutrition-focused approach is widely recognised as a critical adjunct to medical therapy in hypothyroidism and Hashimoto’s thyroiditis, providing meaningful benefits that go beyond symptom control.
Although medication remains the mainstay of treatment, growing clinical consensus highlights that well-considered dietary choices and nutritional repletion significantly impact both short- and long-term outcomes.
A body of research demonstrates that key micronutrients – including iodine, selenium, vitamin D, vitamin A, iron, and zinc – function as cofactors in thyroid hormone production and tissue repair [22]. Even marginal deficiencies in these nutrients can impede metabolic function, intensify symptoms, or slow recovery, especially when left unaddressed over months or years.
Dietary planning begins with understanding individual dietary habits and identifying possible nutritional pitfalls. For example, in areas where iodine deficiency is still found, inadequate intake can exacerbate hypothyroid symptoms or reduce the effectiveness of medication [1]. Conversely, excess iodine might worsen autoimmune thyroiditis for those with Hashimoto’s, particularly for highly susceptible individuals [1].
A focus on whole, minimally-processed foods – including colourful vegetables, nuts, seeds, fish, and lean meats – enriches the diet with antioxidants and essential fatty acids, further reducing chronic inflammation linked to autoimmune flares. High-fibre choices, such as oats, lentils, chia seeds, and fresh produce, are particularly useful (when tolerated) in mitigating constipation, a common issue in hypothyroidism [23].
These dietary strategies also aid in sustaining balanced blood sugar and energy throughout the day, which is crucial as many affected individuals struggle with persistent fatigue and unintentional weight gain.
Applying Nutritionist-Led Dietary Strategies and Lifestyle Adjustments
Yet effective management of Hashimoto’s and underactive thyroid rarely follows a one-size-fits-all blueprint. Instead, a personalised, nutritionist-led strategy is needed to support optimal health and day-to-day functioning.
At the outset, this approach involves a detailed dietary and lifestyle assessment alongside a comprehensive review of blood tests and appropriate functional medicine tests, if appropriate, including gut microbiome or nutrient panels. Identifying and correcting micronutrient gaps – most commonly, low selenium, vitamin D, iron, or B12 – addresses reversible contributors to ongoing symptoms and sets the stage for metabolic improvement.
Nutritionists also help patients navigate confusing food advice by explaining why certain exclusions may help some, but not all, patients. The aim is to build a diverse and enjoyable dietary pattern that supports gut health, immune function, and emotional well-being.
Studies show that interventions such as elimination diets (gluten or lactose-free), energy restriction, and supplementation with nigella sativa (a black seed) were associated with improved thyroid antibodies and hormone levels in people with Hashimoto’s thyroiditis, with the greatest benefits seen in programmes tailored to individual deficiencies and needs [24].
Meal planning, mindful eating techniques, and tips for food preparation are key components of ongoing support. Simple swaps – like increasing oily fish for omega-3s, reducing processed foods, or preparing cruciferous vegetables by steaming – help patients balance benefit and risk without unnecessary restriction [23].
Meanwhile, other studies have found that adherence to a Mediterranean diet, when followed for 12 weeks by women with Hashimoto’s thyroiditis, improved thyroid disease activity markers and contributed to weight loss – even when participants remained on their usual medication doses [25].
Lifestyle modification, closely linked with dietary adjustment, completes the holistic picture. Low-impact exercise not only counters fatigue but also preserves muscle mass, reduces cardiovascular risk, and has been shown to improve psychological resilience in thyroid disorders [26]. Good sleep hygiene helps address the sleep disruptions that many with thyroid dysfunction experience. And stress-management practices, like meditation, guided breathing, or yoga, are strongly encouraged throughout daily life [27].
Managing Hashimoto’s Thyroiditis and Hypothyroidism With The Health Suite
At The Health Suite Leicester, our multidisciplinary structure ensures patients are never isolated in their thyroid health journey. Instead, they are fully supported by a team of medical, nutritional, and allied health experts working closely together to tailor care to each individual’s profile.
Upon diagnosis, a baseline assessment of symptoms, dietary habits, and blood markers is gathered, setting clear treatment goals and identifying modifiable risk factors. Regular follow-ups with in-house specialists enable:
- Close monitoring of nutritional status using tests
- Functional medicine testing
- Adjustments to dietary plans in line with symptoms and test results
- Ongoing tracking of patient progress.
Another key benefit for patients is our integrated education programme. This approach demystifies complex clinical results while giving practical, stepwise advice on meal planning, symptom tracking, and the use of supplements. Dynamic tools, such as digital food diaries, interactive webinars, and one-on-one coaching, foster patient engagement, supporting informed decision-making and confidence in self-care.
Beyond nutrition, The Health Suite promotes wellness through psychological support and chronic disease coaching. This is particularly important during life transitions (such as pregnancy, entering menopause, or major illness) when additional support may be needed to maintain thyroid stability and mood.
For those with coexisting conditions like elevated cholesterol, high blood pressure, or diabetes, the multidisciplinary team develops coordinated treatment plans that address all aspects of health, minimising risk and maximising quality of life .
By combining the latest science with compassionate, patient-centred care, The Health Suite transforms thyroid care from a complex, challenging condition into a journey towards greater empowerment and lasting wellbeing.
Find out how The Health Suite’s personalised, nutritionist-led plans and wrap-around wellbeing support can help manage Hashimoto’s thyroiditis and hypothyroidism.
See how our personalised nutrition and wellbeing support can help manage Hashimoto’s and hypothyroidism.
References:
- Chiovato L, et al. Hypothyroidism in Context: Where We’ve Been and Where We’re Going. Adv Ther. 2019;36(Suppl 2):47-58
- Hu X, et al. Global prevalence and epidemiological trends of Hashimoto’s thyroiditis in adults: A systematic review and meta-analysis. Front Public Health. 2022; 13;10:1020709
- NHS. Underactive thyroid (hypothyroidism). Available at: https://www.nhs.uk/conditions/underactive-thyroid-hypothyroidism/
- Kaur J, Jialal I. Hashimoto Thyroiditis. [Updated 2025 Feb 9]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025. Available at: https://www.ncbi.nlm.nih.gov/books/NBK459262/
- Kaur J, Jialal I. Hashimoto Thyroiditis. [Updated 2025 Feb 9]. In: StatPearls. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available at: https://www.ncbi.nlm.nih.gov/books/NBK459262/
- InformedHealth.org. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. In brief: How does the thyroid gland work? [Updated 2024 May 28]. Available at: https://www.ncbi.nlm.nih.gov/books/NBK279388/
- British Thyroid Foundation. Coping with fatigue. Available at: https://www.btf-thyroid.org/coping-with-fatigue
- Healthline. What’s the Connection Between Hashimoto’s and Hypothyroidism? Available at: https://www.healthline.com/health/hypothryroidism/hashimotos-vs-hypothyroidism#hashimotos-disease
- AADA. Thyroid disease: a checklist of skin, hair, and nail changes. Available at: https://www.aad.org/public/diseases/a-z/thyroid-disease-skin-changes
- Ebert EC. The thyroid and the gut. J Clin Gastroenterol. 2010;44(6):402-6
- Ettleson MD, et al. Brain Fog in Hypothyroidism: Understanding the Patient’s Perspective. Endocr Pract. 2022;28(3):257-264
- Li D, et al. Vitiligo and Hashimoto’s thyroiditis: Autoimmune diseases linked by clinical presentation, biochemical commonality, and autoimmune/oxidative stress-mediated toxicity pathogenesis. Med Hypotheses. 2019 Jul;128:69-75
- Lichtiger A, Fadaei G, Tagoe CE. Autoimmune thyroid disease and rheumatoid arthritis: where the twain meet. Clin Rheumatol. 2024;43(3):895-905
- Szcześniak G, Kozak-Nurczyk P, Dziemidok P. Does concomitance of Hashimoto’s disease and type 1 diabetes affect diabetes control and development of its complications? Arch Med Sci. 2019; 16;17(4):900-904
- Meling Stokland AE, et al. Autoimmune Thyroid Disorders in Autoimmune Addison Disease. J Clin Endocrinol Metab. 2022;17;107(6):e2331-e2338
- Osborne D, Sobczyńska-Malefora A. Autoimmune mechanisms in pernicious anaemia & thyroid disease. Autoimmun Rev. 2015;14(9):763-768
- Sloka JS, et al. Co-occurrence of autoimmune thyroid disease in a multiple sclerosis cohort. J Autoimmune Dis. 2005; 9;2:9
- Popa EC, et al. Hashimoto’s Thyroiditis and Female Fertility: Endocrine, Immune, and Microbiota Perspectives in Assisted Reproduction-A Narrative Review. Biomedicines. 2025; 18;13(6):1495
- NHS. Early or delayed puberty. Available at: https://www.nhs.uk/conditions/early-or-delayed-puberty/
- NIDDK. Hypothyroidism (Underactive Thyroid). Available at: https://www.niddk.nih.gov/health-information/endocrine-diseases/hypothyroidism
- NIDDK. Thyroid Disease & Pregnancy. Available at: https://www.niddk.nih.gov/health-information/endocrine-diseases/pregnancy-thyroid-disease
- Mazur M, et al. Nutrition and Micronutrient Interactions in Autoimmune Thyroid Disorders: Implications for Cardiovascular Health. Pathophysiology. 2025; 1;32(3):37
- Healthline. What’s the Best Diet for Hypothyroidism? Available at: https://www.healthline.com/nutrition/hypothyroidism-diet
- Ruggeri RM, et al. The influence of nutritional intervention in the treatment of Hashimoto’s thyroiditis. A systematic review. Nutrients. 2023;15(4):895
- Shady MA, et al. Impact of Mediterranean diet on patients with Hashimoto’s thyroiditis: a 12-week clinical trial. Eur Thyroid J. 2024;13(4):234-242
- Ahmad AM, et al. Effects of aerobic, resistance, and combined training on thyroid function, lipid profile, and quality of life in women with hypothyroidism: a randomized controlled trial. J Sports Sci. 2023;41(22):2950-2961.
- Wu K, et al. Lifestyle is associated with thyroid function in subclinical hypothyroidism: a cross-sectional study. BMC Endocr Disord. 2021;28;21(1):112
