Small Intestinal Bacterial Overgrowth (SIBO) is increasingly recognised as a significant and often underdiagnosed gastrointestinal condition that affects digestion, nutrient absorption, and overall well-being [1][2].
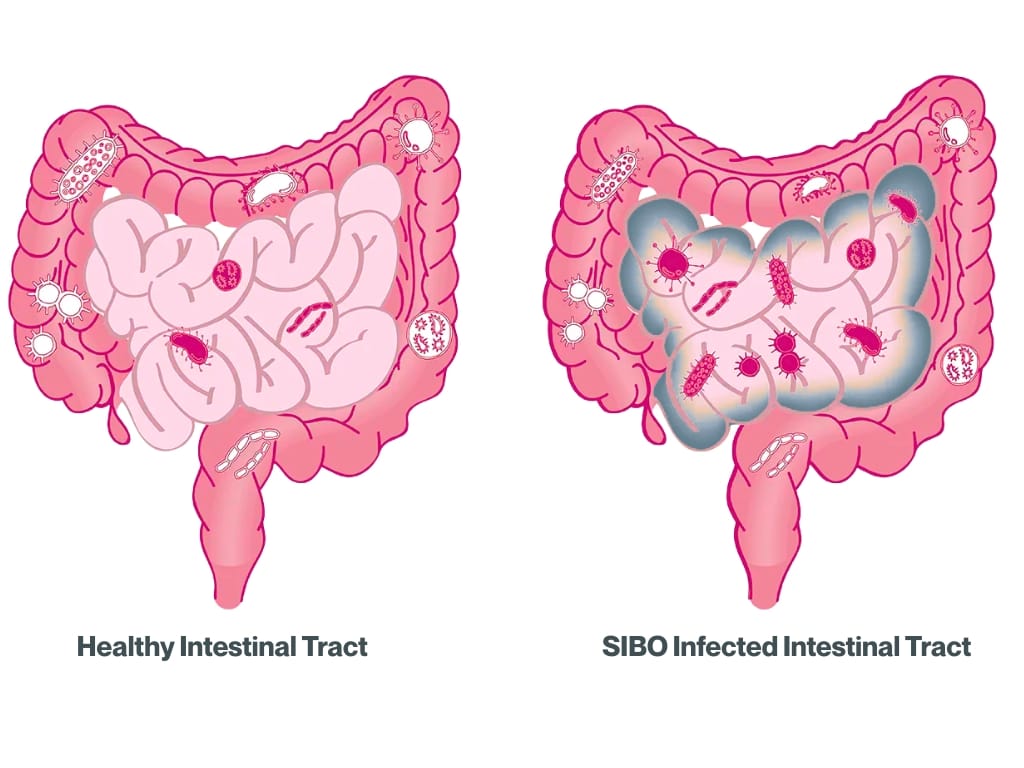
SIBO occurs when bacteria that normally populate the large intestine begin to grow excessively in the small intestine – a region usually home to only a modest number of microorganisms [3]. This imbalance can disrupt gut function and lead to a cascade of symptoms such as bloating, pain, diarrhoea, or constipation, often mimicking other conditions like irritable bowel syndrome (IBS) or coeliac disease [2][3][4].
Understanding SIBO as a Functional Gut Disorder
Recent research suggests that SIBO may be more prevalent in individuals with chronic digestive complaints, with rates particularly high among people with IBS, coeliac disease, or diabetes, as well as those using acid-suppressing medications or recovering from gastrointestinal surgery [2][5][6]. In fact, a study found that SIBO was present in 33.8% of patients with gastrointestinal complaints who underwent a breath test. The presence of SIBO was significantly associated with smoking, bloating, abdominal pain, and anaemia [5].
Women and older adults are disproportionately affected, reflecting the role of hormonal and motility-related factors in disease development [3]. Studies indicate that between 15% and 40% of IBS patients may also have underlying SIBO, contributing to the cycle of post-meal discomfort and bloating common in chronic gut conditions [7].
Importantly, SIBO can recur – especially if the root causes, such as motility issues, low stomach acid, or stress, are not properly managed [1]. Long-term care may be needed, and some individuals require more than one treatment course to maintain remission [8]. Preventing relapse involves addressing underlying factors, maintaining a balanced diet that supports gut integrity, managing stress effectively, and scheduling regular check-ins with a healthcare provider [9].
Recognising Symptoms and Seeking Diagnosis
SIBO symptoms are broad and frequently overlap with other gastrointestinal disorders. The most common include bloating, excessive gas, abdominal pain, diarrhoea, and constipation [1]. Many individuals also report fatigue, nausea, or brain fog – reflecting the systemic effects of inflammation and nutrient malabsorption [10].
Estimates suggest that up to 78% of people with IBS-like symptoms may actually have SIBO when tested appropriately [11]. Because symptom profiles often overlap, diagnosis requires targeted clinical investigation. In some cases, symptoms fluctuate with diet or stress levels, leading to delayed recognition and misdiagnosis. People with coexisting conditions such as hypothyroidism, diabetes, or connective tissue disorders may be at higher risk due to slower intestinal transit [12].
Untreated SIBO can lead to malabsorption of key nutrients, including vitamins B12, D, and iron, potentially causing fatigue, anaemia, and weakened immunity [13]. It may also mask or contribute to the persistence or worsening of other gastrointestinal conditions, such as IBS [14].
One of the most widely used diagnostic methods is the hydrogen and methane breath test, which measures gases produced when bacteria ferment carbohydrates in the small intestine [2]. Elevated hydrogen levels are typically associated with diarrhoea-dominant SIBO (H-SIBO), whereas methane predominance (M-SIBO) is often linked with constipation-predominant patterns.
Other supportive tests may include stool analysis, nutritional blood panels, and imaging to rule out structural issues. An accurate diagnosis is vital for guiding an effective treatment plan, as untreated SIBO can perpetuate ongoing inflammation, nutrient depletion, and bacterial imbalance that worsen over time.
The Nutritionist’s Role in SIBO Management
Alongside the growing understanding of SIBO, there has been a reshaping of how nutritionists and clinicians approach digestion and microbiome health. Once considered niche or secondary to other disorders, SIBO is now recognised as a root cause of persistent gut dysfunction [15] – one that demands a personalised combination of medical treatment, dietary support, and lifestyle modification.
Nutritionists or functional medicine practitioners play a pivotal role in helping individuals manage SIBO through diet, education, and lifestyle support [16]. The primary goal of nutrition therapy is to reduce fermentation, restore microbial balance, and maintain adequate nutrition throughout the treatment process [16].
Many people with SIBO benefit from structured dietary interventions such as the low-FODMAP or Specific Carbohydrate Diet (SCD) [17][18], which restrict fermentable carbohydrates that bacteria feed on. This approach alleviates bloating and discomfort while medical therapies – like antibiotics or herbal antimicrobials – target bacterial overgrowth. Once symptoms stabilise, a reintroduction phase helps pinpoint food triggers and prevent unnecessary restriction.
SIBO can impair absorption of B vitamins, iron, and fat-soluble nutrients [13]. Nutritionists ensure meals include easily digestible proteins, moderate fibre, and healthy fats, alongside supplementation where required. Moreover, techniques such as mindful eating, spacing meals 4-5 hours apart, and avoiding late-night snacking are recommended to stimulate the migrating motor complex (a cleansing wave in the gut that helps to clear out leftover food and bacteria) [19].
Beyond foundational diet work, nutritionists integrate gut-healing protocols that prioritise digestive enzyme support, soothing nutrients like L-glutamine, and anti-inflammatory compounds such as omega-3s and curcumin [20][21]. Over time, gentle prebiotics may be introduced to promote microbial diversity without triggering fermentation. Education also plays a crucial role – clients learn how to balance meals, rebuild tolerance to a wider range of foods, and adopt long-term habits that maintain motility and gut health.
Working collaboratively with medical practitioners and nutritionists who monitor progress, interpret test results in context, and provide the education needed for sustainable recovery and reduced recurrence.
Sustaining Gut Recovery and Resilience
But managing SIBO isn’t just about eradicating bacteria – it’s about restoring gut ecosystem balance and resilience. After initial treatment, many people benefit from a structured plan that focuses on intestinal repair, motility support, and microbial diversity.
Incorporating prokinetic supplements (such as ginger or low-dose erythromycin under medical supervision) can help maintain regular bowel clearance and reduce relapse risk, as recurrence rates can reach up to 44% within nine months without follow-up care [22]. Nutritionists often recommend a gradual return to a diverse, whole-food diet that supports beneficial bacteria through prebiotic-rich vegetables, fermented foods, and polyphenol sources [7].
Lifestyle factors remain key in preventing future flare-ups. Stress management, restorative sleep, and consistent physical activity all promote gut–brain harmony and regulate gut motility. Over time, individuals often see improvements not only in digestion but also in energy levels, mood, and immune resilience.
Beyond dietary and supplement strategies, addressing underlying contributors – such as hormonal fluctuations, thyroid imbalances, or chronic stress – is essential to prevent relapse [23]. Tailored interventions that enhance vagal tone, including deep breathing, meditation, and yoga, can improve digestive rhythm and communication along the gut-brain axis.
Ongoing collaboration between nutritionists, gastroenterologists, and other practitioners ensures that both functional and biochemical factors are fully addressed. Regular reassessment every few months allows for fine-tuning of dietary diversity, microbial balance, and overall gut function, turning short-term relief into a sustainable state of digestive health and long-term resilience.
Managing SIBO With The Health Suite Leicester
At The Health Suite Leicester, our approach to SIBO combines clinical expertise with compassionate, personalised nutrition care. Our specialist nutritionists and functional medicine team analyse test results, review symptoms, and design a holistic plan that targets the root causes of overgrowth, not just the symptoms.
Your tailored programme may include:
- Targeted dietary therapy (such as low-FODMAP or low-fermentation strategies)
- Nutrient repletion to correct deficiencies and improve energy
- Personalised supplement protocols to promote gut healing and motility
- Stress management strategies to support the gut-brain axis
In a friendly and non-judgemental environment, our nutritionists assess any elements of your diet or lifestyle that may be contributing to symptoms such as bloating, fatigue, and irregular digestion. Using evidence-based nutrition, we create a balanced, achievable plan built around your goals – whether that’s restoring energy, reducing inflammation, or improving long-term digestive resilience.
Your SIBO plan is supported through food diary analysis, a 90-minute consultation, and detailed written recommendations, including supplement guidance where appropriate. Through continual progress tracking, education, and empathetic support, we help you rebuild confidence in your body and develop sustainable habits that foster gut strength and overall wellbeing.
With the right combination of medical insight and nutritional expertise, living well with SIBO – and feeling like yourself again –is entirely possible.
Discover more about our nutritionist-led SIBO support at The Health Suite and learn how our integrated approach can help you restore lasting gut health and vitality: Nutritional Therapy at The Health Suite, Leicester.
Get Physiotherapy Relief from Sclerosis Pain Today
Explore our nutritionist-led SIBO support for lasting gut health.
References:
- Guts. Small Intestinal Bacterial Overgrowth (SIBO). Available at: https://gutscharity.org.uk/advice-and-information/conditions/small-intestinal-bacterial-overgrowth-sibo/
- Bures J, et al. Small intestinal bacterial overgrowth syndrome. World J Gastroenterol. 2010 Jun 28;16(24):2978-90
- Sorathia SJ, Chippa V, Rivas JM. Small Intestinal Bacterial Overgrowth. [Updated 2023 Apr 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available at: https://www.ncbi.nlm.nih.gov/books/NBK546634/
- Ghoshal UC, Shukla R, Ghoshal U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy. Gut Liver. 2017 Mar 15;11(2):196-208
- Efremova I, et al. Epidemiology of small intestinal bacterial overgrowth. World J Gastroenterol. 2023 Jun 14;29(22):3400-3421
- Soliman N, et al. Small Intestinal Bacterial and Fungal Overgrowth: Health Implications and Management Perspectives. Nutrients. 2025, 17, 136
- Velasco-Aburto S,et al. Nutritional Approach to Small Intestinal Bacterial Overgrowth: A Narrative Review. Nutrients. 2025 Apr 23;17(9):1410
- Richard N, et al. The effectiveness of rotating versus single course antibiotics for small intestinal bacterial overgrowth. United European Gastroenterol J. 2021 Jul;9(6):645-654
- Velasco-Aburto S, et al. Nutritional Approach to Small Intestinal Bacterial Overgrowth: A Narrative Review. Nutrients. 2025; 17(9):1410
- Rao SSC, Rehman A, Yu S, Andino NM. Brain fogginess, gas and bloating: a link between SIBO, probiotics and metabolic acidosis. Clin Transl Gastroenterol. 2018 Jun 19;9(6):162
- Ghoshal UC, Shukla R, Ghoshal U. Small Intestinal Bacterial Overgrowth and Irritable Bowel Syndrome: A Bridge between Functional Organic Dichotomy. Gut Liver. 2017 Mar 15;11(2):196-208
- Roszkowska P, et al. Small Intestinal Bacterial Overgrowth (SIBO) and Twelve Groups of Related Diseases-Current State of Knowledge. Biomedicines. 2024 May 7;12(5):1030
- Nutritionist Resource. 5 critical nutrient deficiencies caused by SIBO. Available at: https://www.nutritionist-resource.org.uk/articles/5-critical-nutrient-deficiencies-caused-by-sibo
- Losurdo G, et al. The Influence of Small Intestinal Bacterial Overgrowth in Digestive and Extra-Intestinal Disorders. Int J Mol Sci. 2020 May 16;21(10):3531
- Achufusi TGO, et al. Small Intestinal Bacterial Overgrowth: Comprehensive Review of Diagnosis, Prevention, and Treatment Methods. Cureus. 2020 Jun 27;12(6):e8860
- Velasco-Aburto S, et al. Nutritional Approach to Small Intestinal Bacterial Overgrowth: A Narrative Review. Nutrients. 2025 Apr 23;17(9):1410
- Souza C, Rocha R, Cotrim HP. Diet and intestinal bacterial overgrowth: Is there evidence? World J Clin Cases. 2022 May 26;10(15):4713-4716
- Stanford Medicine. The Specific Carbohydrate Diet. Available at: https://med.stanford.edu/content/dam/sm/gastroenterology/documents/IBD/CarbDiet%20PDF%20final.pdf
- Dukowicz AC, Lacy BE, Levine GM. Small intestinal bacterial overgrowth: a comprehensive review. Gastroenterol Hepatol (N Y). 2007 Feb;3(2):112-22
- Redondo-Cuevas L, et al. Do Herbal Supplements and Probiotics Complement Antibiotics and Diet in the Management of SIBO? A Randomized Clinical Trial. Nutrients. 2024 Apr 7;16(7):1083
- SuperSmart. IBS, SIBO, IBD … Understanding chronic intestinal problems. Available at: https://www.supersmart.com/en/blog/digestion/ibs-sibo-ibd-understanding-chronic-intestinal-problems-s241
- Gut Code. Breaking the SIBO replace cycle. Why It Keeps Coming Back & How to Stop It. Available at: https://gutcode.co/2025/02/12/breaking-the-sibo-relapse-cycle/
- Herron, J. G. The Gut Health Protocol: A Nutritional Approach to Healing SIBO, Intestinal Candida, GERD, Gastritis, and Other Gut Health Issues. 2nd ed. 2016. CreateSpace Independent Publishing Platform.
